This page is an open forum for you to share your thoughts with colleagues.
Please consider submitting a brief blog with perspectives about our lives in medicine.
Blog anonymously with minimal descriptive information, or with your name.
Submit to pwp@TCMS.com


Submitted April 2022
by Dr. Quintin Smith
MEDICINE’S GOLDEN AGES
I recently participated in my second Zoom session with third and fourth-year medical students at UTMB, now the John Sealy School of Medicine. It is a Practice of Medicine seminar provided by the school to help give them insight into what specialties they might wish to go. Alumni are asked to answer commonly asked questions as well as offer advice from their perspective, provided from colleagues ranging from early career to retired. Having retired in 2013 after forty-two years in Ophthalmology, you will easily see which category I fit into. In thinking about answers to the “most frequently asked questions” from each year, I am struck by how sincerely the students seek insight and perspective from those who have preceded them. I have been thinking about how this observation relates to the future of Medicine both for these future doctors and those physicians still in the “trenches.”
When I acquired my practice from a retiring colleague, I told him he was retiring at the end of the “Golden Age” of Medicine. Little did I dream of the changes which were to occur in the ensuing years! These future doctors are concerned with many issues but I think “Work-Life Balance” is a priority. At a time when Medicine is struggling with physician “burn-out” and “resilience,” perhaps their concern is well founded. Their training seems to be orienting them toward more teamwork in patient care which may reduce stress. Medical care itself may ultimately be largely provided by paramedical personnel with the role of the physician quite different from what it is today. Perhaps at this time, currently practicing physicians’ “Golden Age” is coming to an end and they will have to accept new paradigms if they are to reach happy retirements. The question is, can today’s physician make the necessary changes? Many practices employ paramedical assistants who deliver significant quantities of care. Undoubtedly, adjustments in lifestyle have been made by physicians as reimbursement levels have changed. Those who have been able to retire have done so and others are considering retirement.
Perhaps the bigger question is whether today’s physicians can accept the inevitable changes, adjust to them and derive pleasure from the remainder of their medical careers? Without doubt, the efforts by our professional organizations to reduce the administrative chaos will help enormously. Physicians still practicing a traditional style of medicine will need to evolve with the times if they are to survive, much like retail businesses faced with the efficiencies and conveniences of their online competition. Hopefully, in the midst of this evolution, they will be able to maintain our traditions of healing. One day most of us may be able to look back at our own “Golden Age,” and for those future doctors, it may be yet ahead.
Quintin J. Smith, MD
qsmith13@att.net

Submitted April 2022
by Dr. Michelle Owens
The Mama Bear Instinct
As a mother of 2 little ones, I’m starting to understand what the mama bear mentality is. Protecting them, advocating for them and doing whatever I can to ensure they have what they need to thrive, survive and enjoy this life.
I started to think about what if we were not only mama bears for our children, but also for ourselves? Imagine - empowering and supporting yourself to be the best that you can be, nurturing yourself and showing compassion and grace in the face of disappointment, advocating for and protecting yourself against toxic situations, people and environments?
This sounds like it could be called fierce self-care.
And all the while we would be modeling these healthy and important behaviors for our children, our partners, our friends, our colleagues, our communities and our world.
If we don’t advocate for ourselves, who else will?
We have to be willing to take care of ourselves, in order to be able to continue to care for others, in whatever capacity that may be.
You have to be a mama bear for yourself. ❤️
Michelle Owens, DO
Physician Wellness Program Co-chair
mowensdo@gmail.com

Submitted, March 2022
Brian S. Sayers, MD
An Officer of the Court
Tony (not his real name) was one of those patients who came to be a friend. I was his doctor for 11 years, guiding him through some very difficult times with a chronic autoimmune disease. He was a handyman, a fly fisherman, husband, father and a man of deep faith. His condition was difficult to control but he always offered a smile as he patiently and hopefully waded through a series of treatments through the years. I’m a terrible fisherman, neither of the two necessary traits (patience and reading the water) coming naturally to me, but it didn’t keep him from giving me flies that he had tied himself, even giving me a handmade bamboo fly rod that to this day sits in my study unused but treasured.
One afternoon my receptionist urgently pulled me out of an exam room, concerned. “There’s a man in the waiting room, a deputy or something, and he wants to see you… he has some papers.” To this day I’m not sure who or what he was other than a messenger of misery. I suppose he was a constable. He handed me the papers, and I vaguely remember a badge, a gun that seemed entirely unnecessary and a decidedly unsympathetic look, a preview of the stress and self-doubt that the coming months would bring.
I hadn’t seen Tony for quite a while and it turned out that he had been diagnosed and quickly passed away with an aggressive malignancy that a plaintiff’s attorney seemed pretty sure several of my colleagues and I should have divined, even in the absence of any signs of it when last seen. This was some years back, in the era before tort reform in Texas, an era where hardly anyone knew a physician who had not been sued at least once. Now it was my turn.
If you haven’t been through it, it’s hard to understand the emotions you go through during malpractice litigation. In some ways it attacks the very core of who you are as a physician, an accusation that you are doing exactly the opposite of what you swore an oath to do and spent all those years training to do well. There was a strong sense of injustice, as I knew I had really done nothing wrong. I was forbidden by counsel to discuss it with friends or colleagues, adding an unhealthy serving of isolation to a plate full of shame and anger. To complicate matters even more, I was simultaneously grieving a man who I considered a generous friend. After a year of silent anguish, second-guessing myself and being suspicious of patients I once felt at ease with, I was as unceremoniously dropped from the suit as I had frivolously been added in the first place. There was a tremendous, but profoundly incomplete, sense of relief. Now even two decades later I still recall those emotions clearly, even as I ironically still treasure the fly rod Tony gave me.
As physicians, we are called on to be many things by patients, and by ourselves. Compassionate, competent, vigilant, intelligent, patient, available, and when lives are in the balance, perhaps even perfect. Litigation, deserved and undeserved, remains a constant threat lurking behind any mistake or just bad luck, but fortunately not as much as some years back. This extreme kind of judgment against us has to some extent been replaced by 100 smaller cuts that we face from criticism from patients or their families, online reviews, peer review, insurance authorization denials, peer to peer reviews, colleagues, employers, practice managers, and at times, most damaging of all, from ourselves. Some of these criticisms are well-deserved, even constructive, and are to be carefully considered as teaching moments, while others are simply based on bureaucracy, greed, frustration or just nastiness. All of them challenge our deep and ultimate calling to bring compassion and love, along with our talents, to each and every interaction with our patients. We have to be careful, through self-reflection and support from colleagues and loved ones, that this type of criticism does not harden us over time in a way that causes us to lose the compassionate calling that a younger version of ourselves set out to pursue all those years ago.
Brian S. Sayers, MD
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com

Submitted March 2022
by Dr. Michelle Owens
What will fill your cup and feed your soul today?
Self-care is not one size fits all. On social media, there are a variety of memes and lists on ways to practice self-care. I’ve noticed these memes and lists seem to primarily contain yoga, meditation, massage, and candlelit baths. Between my husband and me, self-care can look very different, so I’m sure it looks different for others too. Being an Austinite, I think we need a “well-being food truck” with a menu of self-care items listed for people to choose from. Then we can ask “what will fill your cup and feed your soul today?”
Maybe it’s listening to one of your favorite old-school jams or meditating for 5-10 minutes. Maybe it’s calling a friend to say hi or sitting in silence hidden away from the world. It could be practicing gratitude, soaking in a tub with your favorite beverage and show streaming in the background. Or cuddling with your fur baby, bathing in nature, eating fresh pineapple or your favorite sushi, putting pen to paper and letting your feelings flow, or chatting with your therapist. Or maybe it’s a host of other things that aren’t mainstream, and that’s OK. Whatever speaks to you and helps you to refuel is personal; we don’t have to have the same definition of what self-care means or looks like as everyone else. And most importantly, each day and maybe even each hour, we may need something a bit different.
Let’s share with each other what self-care looks like, and maybe we will all be able to add a little something new to our favorite self-care menu.
Michelle Owens, DO
480-734-1110
mowensdo@gmail.com

Submitted March 2022
by Dr. Brian Sayers
Hope Floats
These last two years have affected us all in different ways, but for some, something positive in this long ordeal has been long overdue reflection and a reimagining of our work or relationships. It’s easy to get caught up, sometimes for years at a time, in routines that deplete us, and sometimes we feel unable to make much needed steps towards change, only to feel stuck, even helpless. I hear stories about this from many of our colleagues in my work with PWP and have great admiration for so many who have made much needed life changes that often go against the institutional culture of medicine and our own bad habits. Much needed change snuck up on me when I realized that I was just terribly inefficient with telemedicine in those early days of the shutdown. Appointment slots were lengthened, something I found myself unwilling to undo once I went back to seeing patients in the office. With a lighter schedule my days are less chaotic and stressful, and I came to love my work again. I’m nearer the end than the beginning of my career, my kids are off the payroll and I’m self-employed so admittedly I am able to make changes that will make my work more sustainable in the years to come that not everyone can. Still, I have to shake my head that it took me so long to realize the trade-off is well worth the bottom-line sacrifice.
To further confound my financial planner, we bought a little farm an hour or so from town during the shutdown. It’s been a steep learning curve of wells and septic fields, irrigation systems and permits, spiders and snakes, but I fell in love with the old farmhouse and the olive grove that covers much of the property. The previous owner planted 200 olive trees years ago that flourished until the big freeze of 2021 killed off about a third of them, most of the rest severely damaged. This past year after we purchased it most of them have started growing back as shoots, four or five feet by now. It’s a metaphor for our own recovery from these last two years, but I’ll set that aside for now. Relaxing there and not worrying about patients quickly morphed into worrying about the grove, but it’s different and there is satisfaction in watching life being breathed back into the place, ever so slowly. I wander and tend to it weekends and have made each of my grandchildren adopt a couple of the struggling trees, measure and talk to them when they visit.
It’s an experience that has made me reconsider hope. I can imagine how people who farm or ranch for a living center their lives around hope each year, just as we do when we look at our children or grandchildren, or a patient, friend or family member who is struggling or ill, or when we wish our workdays would nourish rather than exhaust us. Hope is the underlying current in optimism, the wind in the sails of our lives, and without it we are set adrift. These last two years have given me a chance to reconsider what I hope for, sometimes pray for, and what I should let go of.
The drive to the grove is about the right distance to unwind and, for the moment at least, leave the worries of Austin behind. About 15 miles from my turnoff, I pass by Smithville. There is a sign on the highway announcing “Smithville, Home of Hope Floats.” It was a popular movie filmed there that most of you have seen, a story about humility, divorce, childhood trauma and death of a love one, but in the midst of it, from the ashes, a new family, happiness, wisdom and hope emerge. I watched it again recently, trying to remember the line in the movie that the title comes from. It is at the end when Sandra Bullock’s character notes, “Beginnings are scary, endings are usually sad, but it is the middle that counts the most…Just give hope a chance to float up, and it will...” The sign is badly faded and whizzing by a bit above the speed limit all I see each time is the reminder that “Hope Floats.” And that is enough.
Brian S. Sayers, MD
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com

From the Other Side
As I sit at the bedside of my grandmother, she is on her final journey out of this world and I am reminded that life goes on despite the hardships we navigate.
Golden Girls is playing in the background – a show I grew up watching with her every time I’d visit.
I am a hospice physician – my day job is helping to ease suffering and allowing for a peaceful death. Yet being on the other side as a family member is the hardest thing I’ve ever done.
I reflect back on my journey into medicine and how I ultimately decided on pursuing a career in hospice and palliative medicine. The experiences throughout my education colored my path to be able to navigate this exact moment. I truly feel I’ve been preparing my whole life for this moment – to truly advocate for my grandmother and know what to ask for, to comfort my family and gently deliver the news that she’s dying, to understand what terminal delirium and agitation look like and hope to give myself the compassion and grace I tell my patient’s families to give themselves when faced with a similar situation. Yet knowing all these things, I still struggle.
I am in awe of the beauty of the gift of time. How fleeting it comes and goes. Although I am reminded daily in the work that I do that we are not promised tomorrow, this impending loss is not any easier.
Our life experiences shape us into who we become and our losses remind us of the beauty of being human, knowing suffering, and holding love and loss in tandem. I will forever be changed after experiencing this loss. I now understand even more how devastating and debilitating loss can be.
My grandmother’s death will make me a better physician, mother, wife, daughter and friend. As they say, it’s better to have loved and lost than to never have loved at all.
Dedicated to my grandmother, Blanche Beverly Owens (1932-2022)
Michelle Owens, DO
Co-Chair, TCMS Physician Wellness Program
mowensdo@gmail.com

RECLAIMING JOY
I watched as her face glowed with excitement as she told me her MCAT scores. Her prospects of being accepted into medical school had just increased. This was her third attempt at the MCAT. She is a patient care technician who works in my hospital. We shared the same patients on many occasions. She had made efforts to seek my company whenever I rounded. As I looked at her face in her excitement, I remembered my own. Unknowingly, she gifted me with the memories of that time when I fought to enter our profession. I immigrated to the US at the age of 8. English was my third language. Because of this language barrier, I struggled with the MCAT. It was not the only barrier. My birth country and culture did not support women in higher education. In addition, my parents were poor immigrants themselves and I had to work my way through college and medical school on my own. Yet, I was not deterred. Acceptance into medical school was one of the joyous highlights in my life because it had been such a struggle.
Somewhere along the way, like so many of you, I forgot all of that and lost my joy as a physician. The workload, long hours, heavy responsibilities, electronic records, and attempts to meet impossible metrics squashed my love for medicine. Fresh from training, I had joined 3 other men in an internal medicine practice in Kansas. I remembered the oldest of the 3 men in his 70s said to me on my first day of practice, “I am sad for you joining medicine these days with such a broken system.” Over the next 2 decades as a hospitalist, I realized how true his words were. These past 2 years during the pandemic worsened my attitude. Going to work every day felt heavy. I vacillated between anger and sadness.
In sharing her new MCAT scores and her excitement, my young friend suddenly brought me to a place of gratitude. I remembered the difficulties and remembered where I was and where I am now. It was as if a switch was just turned on. I remembered the excitement of scrubbing in for surgery for the first time, delivering a baby for the first time, placing a central line for the first time, intubating a patient for the first time, and being called “doctor” for the first time. My eyes were wide open. My mind had the humility of a beginner. Back then, no one could take my joy away.
So, what happened? I could name all the things that I feel took away my joy for medicine. Trust me, it would take a whole lot more than these pages could hold. I am not so “Pollyanna” that I do not see the destruction of our health system. Nor do I deny that anger doesn’t come up when I witness the atrocity physicians must go through to care for their patients. However, I am at a place where I am sick and tired of being sick and tired. I have decided no one can take away my joy. I am no longer willing to give the power and control to another or a system. I get to reclaim it.
I started to reclaim my joy of medicine by remembering what brought me here in the first place. For me, it is the art of medicine itself and the connection with patients and colleagues. I felt thrilled to be able to diagnose the unique unilateral hyperhidrosis and vertigo associated with a stroke. I “get to” sit down with a stage IV ovarian cancer patient who failed treatment as she taught me the art of dying. I get to brainstorm with colleagues on challenging medical problems and finding shared vulnerabilities of “I have no idea what this is.” I consciously chose facilities and hospitals that value my work. I chose practice partners that share the same philosophy in medicine and support my need for time away. I cut hours of working so I can tend to my own healing. It is in these things that I find joy while still working in a broken system. I have learned after nearly 3 decades in this profession, there is never a right time to make changes. If I don’t do it now, it may never happen. As a physician working in acute care, I learned life is fleeting.
My young friend was accepted into the medical school of her choice. She did not have to say anything. I saw it on her face. I saw and felt joy.
This quote by Josh Shipp summarized it all for me: “You either get bitter or you get better. It’s that simple. You either take what has been dealt to you and allow it to make you a better person, or you allow it to tear you down. The choice does not belong to fate, it belongs to you.”
Dr. Anna Vu-Wallace
annavuwallace@gmail.com

Friendship
This weekend I was putting together some promotional material to introduce TCMS members to the PeerRxMed program, a buddy system to help physicians connect and support each other one-on-one on an ongoing basis. As we have tested the program, I found myself reconsidering the importance of connection in general and more specifically the nature of friendship. It’s an important topic these days and much has been written about the high percentage of doctors who feel isolated, the “Loneliness Epidemic,” and the known physical, professional, and emotional consequences of isolation that have been extensively studied recently.
Isolation from friends and colleagues is not a new problem. In fact, some authors argue that physicians by the nature of their training and work are more susceptible to it than most, and for many maintaining connections has been made worse these past two years. Maintaining, let alone nurturing or developing, new friendships and meaningful, healthy connections takes effort, time, emotional energy, and more recently, not just a little imagination. With so much at stake in having not just acquaintances, but true friends in our lives, it’s worth considering the nature of friendship and what friends should be for one another. David Whyte describes friendship and the consequences of neglecting them this way:
“…the ultimate touchstone of friendship is not improvement, neither of the other nor of the self, the ultimate touchstone is witness, the privilege of having been seen by someone and the equal privilege of being granted the sight of the essence of another, to have walked with them and to have believed in them…on a journey impossible to accomplish alone. An undercurrent of real friendship is a blessing exactly because its elemental form is rediscovered again and again through understanding and mercy.
...a diminishing circle of friends is the first terrible diagnostic of a life in deep trouble: of overwork, of too much emphasis on a professional identity, of forgetting who will be there when our armored personalities run into the inevitable natural disasters and vulnerabilities found in even the most average existence.”
We ignore our friendships and their vital importance in our lives at our own peril, both individually and as a society. Mother Teresa observed that many of the world’s ills are a result of having “forgotten that we belong to each other.” Deeply connecting and sharing not only life’s joys but also our challenges and fears is not a sign of weakness, rather a profound form of personal and collective strength.
Whether you participate in the PeerRx program or not, find ways in your busy days to connect with friends and colleagues on a regular basis. You will absolutely make a difference in their lives, but also consider, as Gregory Boyle notes in Tattoos on the Heart, that this act of friendship - of kinship - is “not serving the other but being one with the other.”
Brian S. Sayers, MD
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com

Standing on Holy Ground
One of my favorite passages from sacred writings is the story of Moses, still tending his father-in-law’s sheep, an ordinary day in an ordinary place, suddenly encountering God, the ground he stood on now consecrated into holy ground, admonished to “Take off your sandals, for the place you are standing is holy ground.” All of the world’s religions speak of holy ground. For Muslims, even the simplest prayer rug in the humblest of places becomes holy ground to commune with Allah. Buddhists may have a transcendent experience at a stupa. The concept of holy, or sacred, ground transcends religion and in a secular sense people commonly find themselves encountering a different spiritual plane in all kinds of places. The experience may sneak up on you, but requires open eyes to be receptive to it.
Some years back, my wife had an appointment with a specialist at Southwestern in Dallas where we would receive more news about a diagnosis that would forever change our lives in so many ways. While she was waiting to be seen I went back to the medical school auditorium where I spent so many transformative hours all those years ago. The room had many technology upgrades over the years but it was still much the same. I considered my own time there and the fact that the doctors Maryann was seeing next door all would have either trained or taught in this same room, and I had a sense of an almost mystical nature of this ordinary room, of all the lives changed for those who passed through its doors. Similarly, a patient of mine recently described such a feeling when visiting the military cemetery at Normandy. The se spaces can outwardly be ornate or very ordinary, ground that becomes extraordinary and carries with it a moment in which we seem to commune with something beyond ourselves – a favorite place in nature, working in a food bank, quietly nursing a baby.
So, how might we describe holy ground in ways that may be recognizable, even familiar, to all of us regardless of whether we appreciate its presence with religious, spiritual, or purely secular eyes? Some describe it as a “thin place,” something the Celtic tradition describes as a place where the space between the material and the divine becomes very small, where the concrete merges with the infinite, where our tangible, practical world is suddenly enveloped with mystery and intangible truth. Where, for a time, we feel untethered and are united with a hidden world and souls around us. As with Moses, or the prayer rug, the stupa, even an auditorium, the terrain itself may be ordinary, but what happens upon it, or what it comes to signify makes it sacred.
In health care, presumably there was an original sense of calling to heal, a calling that you answered years ago and still follow. For all of the things that get in the way of us pursuing it well, we are still incredibly privileged to inhabit the holy ground on which we meet our patients, people on a common journey with us, who literally and figuratively bare their bodies and souls before us, with trust – with an assumption that we will come to them with humanity, compassion and fidelity, to stand on this ground, and as we do it we agree to leave behind the encumbrances and baggage that we all carry. For the moment, we leave it all at the entrance to this sacred and mysterious space.
Pause at the door, take a cleansing breath, then enter the exam room, or hospital room, ER cubicle, or operating room. Take off your sandals, you are standing on holy ground.
Brian S. Sayers, MD
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com
Photo credit: Ashley Yeaman, Focus Magazine
The Covid Chronicles…
Submitted November, 2021
by Dr. Leslie Cortes
COVID Apocalypse
Almost from the beginning of the pandemic, I have referred to it as the COVID apocalypse. I use the word apocalypse in both its secular meaning of disaster or catastrophe as well as in its original meaning from its Greek root for uncovering or revealing. With the first meaning, I refer to the toll of illness and death as well as the disruptions of societal functions and global economics that the pandemic has caused. The latter meaning refers to the unmasking of things both good and bad.
Most of the good that the pandemic has revealed has been at the individual level, I think – compassion, service, altruism, and self-revelation – a better understanding that we each have of ourselves and what is important to us. Much of the bad revealed has been at the organizational and structural level – inequity, inequality, greed, and callousness. These things have always been with us, but the apocalypse has laid them bare. It has revealed how politics taints public health decisions, how political rhetoric taints the decision-making of individuals who profess to live by the Golden Rule as well as the decisions of our public institutions that profess to serve us all.
It has pulled back the curtain on pretenses to reveal how corporations that claim to be engaged in making us all healthier readily put profit above probity. It has revealed the hypocrisy of expressions such as “essential workers” when they are used to apply to healthcare workers and first responders but not the workers who keep our pantries stocked, our utilities on, who teach our children, and who make life seem normal despite the ongoing conflagration. These are the workers who make it possible for those of us, more privileged, to work from home, shop from home, and otherwise minimize our exposure to potential infection.
I am among the privileged because my wife and I are retired with a secure income; many Americans are not. I am among the privileged because my wife and I are vaccinated; most of the world is not. I am among the privileged because of an accident of birth, a helping hand from many I have met in life, and an occasional fortunate decision rather than because I deserve it. For these things, I am grateful.
Leslie L. Cortes, MD
llcortes55@gmail.com
Submitted November, 2021
by Dr. Michelle Owens
“What are your goals of self-care?”
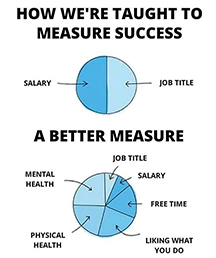
"This graphic made me say “Yes! Yes! Yes! 1000% this!”
In hospice and palliative medicine, one of our most common interventions is a goals of care conversation – like an appendectomy for a surgeon or a tonsillectomy for an ENT. A goals of care conversation explores what patients value most in life and helps to guide their medical care in a way that meets their specific life needs.
In the 5 years I have been practicing, I’ve realized that these goals of care conversations actually translate across most areas of life – not just at the end. In fact, you could consider many of the questions asked could be part of a “goals of self-care” conversation. What better way to guide our decisions and provide a better measure of what a successful life looks like?
Think about this for a moment:
Instead of asking “what are you willing to go through to get more time?” to a person living with serious illness, we might ask ourselves, “what are you willing to go through in your work life to be able to maintain your home life balance?” Or “what are your work life and home life non-negotiables?”
The question “what do you want to do with whatever time you have left?” is appropriate for all of us at any time.
The questions “what brings you joy?” and “what gives you strength during hard times?” are also appropriate for us to reflect on.
The only things we are promised in life are change, taxes, and death. We are tasked with being good stewards of our energy and living this life to its fullest.
What other questions could we ask ourselves to ensure we are living the best-balanced lives that we can?
I encourage you to start your own goals of self-care conversation.
Michelle Owens, DO
mowensdo@gmail.com

The Covid Chronicles
Submitted by Dr. James Marroquin
November, 2021
On a winter trip to New Mexico earlier this year, our family hiked to a frozen lake. My sons Elijah and Micah threw rocks at the water and watched the surface crack. They then hurled sheets of ice they created, shattering them across the lake. Even as the cold turned their hands beet red, they couldn’t get enough of this chilly activity.
Watching their carefree sense of wonder and fun, I reflected on my very different mindset in middle age. These days I feel the need to ensure every moment of my day is purposeful. When a gap opens up in my schedule, my first thought is how it can be usefully spent. A positive way of framing this is that I’m being a good steward of my time. But there are less flattering interpretations of this quest for perpetual productivity. Am I seeking to make myself feel important? Am I distracting myself from uncomfortable realities?
To become physicians, we put in long hours, sacrificing time with friends and family. We were conditioned to make work our highest priority. For many of us in clinical practice there are always more tasks to be done. And the portability of the EMR enables us to continue the grind even after we’ve arrived home.
It’s challenging to put limits on our work--to set apart and protect time to rest, play, connect, and savor our lives. Some doctors unfortunately don’t have control of their work schedule. But even if we do, it’s easy to view these “non-productive” parts of our lives as less worthy of our time and attention. With growing levels of burnout worsened by Covid, it’s vital physicians spend our days in ways that enable us to thrive in our lives and not just our work.
For me that’s included around ten minutes every morning outside gazing at the sky. I notice the trees swaying, clouds shifting, birds chirping, wind chimes clanging, and the sun slowly rise. Sometimes my golden retriever Hunter even comes by for a pet.
I’ll end with a powerful exercise from the social scientist Arthur Brooks. First, imagine yourself in five years. Picture yourself as happy, whatever that means for you. Next, list five things that made you happy five years from now. Place them in order of their importance in bringing you joy. Lastly, ask yourself how to best manage the two most important priorities on your list. How can you invest in them to enable them to grow and flourish?
Dr. James Marroquin
jamesmarroquin@gmail.com

Submitted October 27, 2021
In These Silent Days
I’ve been trying to make sense of anonymously submitted surveys that colleagues fill out when they access the TCMS Safe Harbor Counseling Program. With over 1000 counseling visits funded so far, there is a lot of data, and I am poorly equipped to analyze it. Two of the questions ask: “Please rate your satisfaction with your work,” and “Please rate your satisfaction with your relationships outside of work.” We’ve seen over 97% of respondents express satisfaction with the therapy they have received, but no convincing data that they are accessing counseling primarily because of dissatisfaction with work or relationships.
My original thesis debunked, why then do physicians access counseling? It’s a question worth considering as we’ve seen a dramatic rise in utilization of the program during the pandemic, especially starting around the first of this year and again in August after so many months of challenge.
I’ve asked psychiatry colleagues and therapists their perspective on why our colleagues seek therapy. A therapist I trust pointed out something that should have been obvious. Many of our colleagues come to therapy not just with stressors from work and relationships, but rather, in this unique and prolonged time of challenge, they come to therapy in the midst of a sort of “stalled discernment,” a sense that change is needed, but without clarity of what that should be or how to pull it off.
For most, these many months in pandemic, especially the early ones, have been times of upheaval and uncertainty, a vague anxiety and loss of balance ever present in the background of our work and family life. But more importantly, it has been a time that cries out for us to identify foundational things that make us whole and open our hearts. Intermingled with the chaos have been moments or days of reflection and reassessment. For many, it has been a time of discernment as we consider where we were in our frenzied pre-shutdown lives and how we might reimagine our future. A time to assess what is nourishing and life-affirming and what must be left behind. The results are all around us. In our own lives and those of countless colleagues there has been a realignment of family life, and in the workplace, unprecedented numbers retiring, leaving clinical practice, changing practice settings, or otherwise trying to make their work sustainable for themselves and their families.
Singer/songwriter Brandi Carlisle calls this time, “these silent days,” noting that “either way, I lose you in these silent days…” perhaps meaning we will all be different in some way or another as a result of these past months. Shedding the old is always a part of becoming new. Writing in the Annals of Internal Medicine, Dr. Ranna Anwash observed it in a similar way:
“If we are to find a way to live our values in these demoralizing conditions, we must hold on to what is nonnegotiable in ourselves—not because it will heal our patients but because that is the only path back to ourselves. And, yes, it will be a different version of ourselves that we meet on the other side of this. One that no longer believes in neat and tidy happy endings. Someone with perhaps a little less faith and who is still in need of healing, but potentially—hopefully—someone we recognize.”
Henri Nouwen described discernment as “reading the signs of daily life,” of seeing − and recognizing − ordinary and extraordinary events of life as signposts for both the present and the future. Discernment goes far beyond decision making. It is about rediscovering core beliefs and values, joyful living and the things that breathe life into us, then making them the defining movements in our lives, something at once difficult and essential.
Brian Sayers, MD
bsayers@austin.rr.com

The COVID Chronicles
Submitted by Dr. Kim Wheeler
October 2021
Small Town Covid
In March 2020 I joined a TMA Teleconference regarding a virus called COVID19 that was in China. The TMA called all members that night with an update. As I listened, I almost dropped the phone as we were notified that the virus was among us and would become “The pandemic of our lifetime.” We were also notified that PPE and testing supplies were scarce so in essence “Good Luck.” And the TMA was correct. COVID19 had arrived. Within days our small-town family medicine practice had implemented telemedicine, put strict office mask and sanitation protocols in place, obtained as many PCR swabs as possible to start curbside testing, and went to two shifts so if one shift had to quarantine the other shift could take over. We worried that we would become infected and infect our families. We went to work every day and never missed a beat. In December, we were overjoyed as we were offered vaccines. There was a sense of relief that we could do our jobs safely now. We provided hundreds of vaccines to our patients. In June, the CDC was giving a positive outlook and we were feeling hopeful.
Then July hit. We started seeing a surge of COVID that was worse than 2020. We were tired and unprepared for seeing anything “worse.” By August we were booked a week in advance and had dozens of “COVID positive” patients calling daily for appointments and infusions. Most were unvaccinated, but we were alarmed to see vaccinated patients testing positive as well. By October 2021 we have had hundreds of patients infected with COVID19, many have been hospitalized, and unfortunately many have died. We’ve seen families lose multiple loved ones. It has become part of our lives, part of our daily discussions with patients.
BUT . . . w e are becoming hopeful again. Vaccines are easily accessible and boosters have begun. Children under 12 will soon be able to get their vaccines. There is talk of a pill for COVID that is being developed by Merck. Many unvaccinated patients who got COVID during the surge now plan to get vaccinated. There is a faint light at the far end of this tunnel. We cannot give up. We have come too far. We care too much. This is what we do.
Kim Wheeler, MD
Lockhart Family Medicine
wheelerk4@yahoo.com

Submitted by Dr. Tyler Jorgensen
October, 2021
Seeking Still Waters
Whitewater paddlers make it look so easy—staying upright in raging waters, navigating huge swells, leaning and cutting hard at just the right time to avoid dangerous obstacles. And when they do flip upside down, they are able to pop themselves right back up. It’s a marvel. But no matter how expertly they paddle, they always have to respect the power of the water. The moment they let their guard down and get too comfortable, they can make a careless and costly mistake.
We physicians do the same. We take an inherently dangerous, complex, and difficult discipline and learn to practice it as an art. We learn how to navigate tricky diagnostic pathways, respond rapidly to changing clinical conditions, and try to stay emotionally upright while riding successive waves of an ongoing pandemic. On our best days, we glide through the whitewater of medicine with style and grace. But if we let our guard down and get sloppy, we can end up making a careless and costly mistake. Who of us isn’t fatigued by constantly having to be on guard in the whitewater?
I have been thinking a lot about paddling lately. Getting out on the water has remained a source of wellness and renewal for me since residency. I enjoy just about all paddle craft. Sometimes it’s sitting inside a skirted kayak at the level of the water and flipping upside down only to pop up again—a sort of natural baptism that puts us in fellowship with the ducks and the turtles. Or maybe it’s hopping on a stand-up paddleboard on Lady Bird Lake, and immediately feeling carefree, relaxed, and untethered. Other times it’s paddling a gracefully-curved canoe with a friend, such a timeless and grounding adventure of shared effort and striving, shared wonderment, and sometimes shared suffering!
My current kayak is an unusual one—a black, open-hull, lightweight carbon-fiber downriver racing boat. At nineteen and a half feet long and twenty-one inches wide, with gunwales just a few inches off the water, it is super tippy. I have unintentionally flipped and flooded it many times. This boat was designed for racing down the San Marcos River, but I am still just trying to keep it upright in still water. To do so I am learning how to engage my core at all times and work on balance. No false or careless moves. It forces me to slow down and focus on my breathing and movements in ways no other boat has. I am enjoying the challenge.
Regardless of paddle craft, I have yet to spend a day on the water with a friend that didn’t result in fantastic conversation and deep connection. Hours on the water in nature together steadily take us to unhurried and thoughtful exchanges, along with potent periods of shared silence. Neither have I spent a day alone on the water that didn’t result in greater inner peace and calm. Meditation, gratitude, joy, wellness.
Here in Travis County, we are surrounded by waters. If you need a new wellness strategy, can I recommend getting out on the water? Whether it’s Lady Bird Lake, the San Marcos River, or a quiet section of Barton Creek, the water always buoys me up, helps me find balance, refreshes me, and draws me into deep connection. It can do the same for you. There is even growing neuroscience to show that bilateral alternating movements (like paddling) can help our brains process trauma. And we all know the countless benefits of time in nature.
As thrilling as whitewater can be, these days I find myself seeking still waters. Even while at work, in the midst of busy whitewater days, I am coming to find moments of still water. If I seek out and recognize these moments, slow myself down and work on my breathing, I re-discover the balance and form to keep me paddling downstream, staying upright in the everchanging waters of practicing medicine. I hope to see you on the water.
Tyler Jorgensen, MD
tylerscottjorgensen@gmail.com

By Dr. Brian Sayers
Harvest
A long time ago, I spent three years in Albuquerque doing an internal medicine residency, years spent at the county hospital, a Public Health Service facility serving the Navajo and a regional VA. Those were good years, a time of learning how to care for people − once I figured out how to keep them alive. Strange as it sounds, one of my best memories of those days was eating on the patio of the VA cafeteria. They made the most amazing green chile stew, full of chile softened by hours of simmering, with pork, vegetables and spices thrown in. I would look forward to lunch throughout morning rounds. We sat together at a communal table, sharing stories about the strange cases and people we were caring for, quirky attendings, stupid mistakes, saves and codes, turfs and lack of sleep. We were all navigating southwestern and Navajo culture with varying degrees of success. We were learning the importance of understanding people’s culture in order to care for them successfully.
I soon learned that the chile harvest was the pulse of life in New Mexico. Fall in northern New Mexico was all about hot air balloons, the chile harvest and the communal celebration of both, with morning skies full of colorful hot air balloons rising in the high desert sunrise. Throughout the state, chile farmers would proudly bring their harvest to market in tourist towns, small villages and roadside stands, ready for cooking or decoration.
In the southern part of the state, commercial growers produced huge crops, mostly bound for Louisiana and the inside of hot sauce bottles. But in northern New Mexico, the norm was small family farms that have grown chile for many generations, the hard labor of growing chile an integral part of the culture, the rhythm of daily life and an ingredient in almost every meal. These small family farms were largely owned by folks with deep roots there, many direct descendants of Spanish colonialists with strong Native American heritage. They have worked the land and passed it and their way of living down through uncounted years, their hearts beating in rhythm with the land and the climate, with the very soil that they labor in. Deep within their culture is an identity with that soil, with its innate mystery and value, a sense of its holiness. Even a modest harvest is a great source of pride and a cause for celebration. As one chile farmer is quoted in Carmella Padilla’s The Chile Chronicles, “My mother always used to say, ‘If you plant it with joy, it will grow.’”
One day I was eating a late lunch after a night on call. Our attending was an older man who inhabited a wonderful, open hacienda style home outside of town in the foothills of Sandia Peak. At the end of each rotation, he would host his residents and students, introducing us to New Mexican wine as we looked over the lights of the city. He exuded calm, a trait much needed in those days, and one I have tried unsuccessfully to emulate in the years since. He walked onto the patio, bowl of stew in hand and sat down with me.
One of our admissions the previous night was a poor, elderly chile farmer from Chama, his large extended family having brought him all those miles for care at the VA. It was an impressive sight, this tribe of modest laborers all gathered as a family to stand vigil. He had told me about his little farm and his family that night and I related some of it on rounds. “I’ve always admired people like him,” my attending said. “When we are at our best, we are more like them than you might think, grounded in culture and family. When you leave here, you’ll take a new culture and a new family with you.” I’ve thought about that offhanded bit of wisdom dispensed over a bowl of green and have considered its meaning in the years since. Those chile farmers were deeply rooted in the soil, the rhythm of the seasons and their heritage. It binds them together, gives them purpose and faith. Along with my own heritage of faith and family that I brought to New Mexico, I added new roots, the timeless culture of medicine and healing, and had been given a new family, just as you were on your own unique path. That sense of culture and family, that calling, will always be there, waiting for us to return even when we wander or forget, drawing us back, in some form or another, to what we were meant to do.
Brian S. Sayers, M.D.
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com
Submitted September, 2021
by Dr. Michelle Owens
Gratitude
During a well-being debriefing with my work family this week, the strategy of practicing gratitude was shared as a way to practice self-care to be able to navigate these continued times of uncertainty and acute on chronic stress.
This resonated with me deeply as earlier in the year I had adopted a gratitude practice with my husband. Every evening, right before bed, we take turns sharing 3 good things that happened to us during the day. Often times they would be similar and related to our young children. We found it to be a nice way to end the day and drift off to sleep with comforting feelings instead of exhausting thoughts of one of the many worries or stresses of the day. I also noticed I slept deeper and was more rested in the mornings.
I’ve heard other colleagues share similar gratitude practices - some starting their days off by reflecting on 1 good or meaningful thing that happened the day before; others reflecting on 1 meaningful interaction they had with a patient or family that day on their drive home from work; and others practicing daily gratitude journaling. They all shared how impactful their gratitude practice had been on their overall well-being, and many shared that they look forward to that practice each day.
This is not a novel idea and the field of positive psychology has focused on the impacts of practicing gratitude with happiness for years. It’s not surprising that people who routinely incorporate the practice of gratitude in their lives report feeling happier, more optimistic and with an improved well-being. Some studies have shown increased exercise and fewer visits to physicians, as an association with the practice of gratitude.
There are many ways to practice gratitude and none are superior to others - it’s truly what speaks to you and ultimately fills your cup. Gratitude is a salve for our emotional wounds.
What ways do you incorporate the practice of gratitude in your life?
Dr. Michelle Owens
mowensdo@gmail.com
Submitted September 2021
By Mark Rosen, M.D.
Seeing the lost and overwhelmed look on one of the new ICU nurses reminded me of my internship.
My high grades came easy to me - until medical school. Suddenly I found myself surrounded by others at least as smart as me. Most of them had a hard work ethic while I was always able to manage without much studying. I continued to enjoy the campus and city life at my prestigious medical school, with grades well in the middle of the pack.
I applied to 13 top internship programs plus two safety nets. I got into #14. I was devastated. This was in Miami, Jackson Memorial Hospital, and some of the wards were not even air conditioned. I was so naïve back then. I had no idea that to get into a top internship, you needed to get references from top academicians, and you need to have done research for at least one of them. Not me.
My first month was ICU, where the resident just had one intern and I was protected for the most part. The second month was the Medicare ward, old and sick. My first night on call the ER doc admitted to me a patient with pulmonary edema. I went to the ER and saw a cachectic man on a Bird respirator (as if anyone reading this knows what that is), no edema, no rales. Bed, IV pole and ventilator. It was my responsibility to move him to the floor? How? Do I have to grow a third hand? You know us guys, we don’t like to ask for help or directions. But I had no choice. Turns out we were to call respiratory therapy and they move the vent. I got the patient tucked in upstairs and figured out he had decompensated COPD. Dry as a bone. My first big lesson: don’t trust what other doctors or the patient tells you about the diagnosis. It’s a good place to start but make your own decision.
Things went downhill from there. I was sure I would kill someone from missing an obvious diagnosis (we learned thousands of them in med school) or ordering the wrong medications (ditto). I became depressed with what I now recognize as PTSD. Couldn’t sleep, no appetite. Dreaded going to work. Tachycardia whenever I was not at work and heard a siren.
My medical school rotations, being at a tertiary referral center, gave me little chance to make decisions. I’d be the fourth or fifth doctor to see the patient, and everything was known and planned by that time.
I told my housestaff director that I was going to have to quit. He refused to accept this and told me to take some more time. I had an elective coming up and wouldn’t be faced with decisions or night call for a month. I saw a therapist. Wasn’t given antidepressants or antianxiety meds, not sure why. I sure needed them.
Month 4, back on general wards. Night call, asked to see one of my fellow intern’s patients with abdominal pain. He had a board like belly. First thought, call surgery. Second thought, he will ask me what does the CBC and abdominal film show? So I ordered those. Free air under the diaphragm, called surgery, off to repair a perforated peptic ulcer.
Even now I still tear up when I tell this story. I realized that I did know what I was doing. There were only a few medications for pneumonia, not thousands. There were only a few diagnoses we had to deal with daily. The few exceptions were sent to specialists, discussed in morning report or grand rounds, and got treated appropriately.
My symptoms resolved and I finished my training without further such problems.
In retrospect, I was thrown into the deep end without knowing how to swim. If I had been accepted at one of those top internships, I’d still be dog-paddling. I truly believe that I am a much better clinician now having had the training at Jackson Memorial rather than elsewhere.
Which is sort of the story of my life. Without exception every disaster, calamity, disappointment in my life has turned out to be the opening to something better. Sure, part of this is just my attitude about life. If I’m on vacation and miss a plane, so what? I’m still on vacation. Read a book in the airport instead of on the beach, who cares?
I met my wife of 47 years in Miami. Which wouldn’t have happened elsewhere obviously.
I’ve been practicing medicine for 44 years. From the start I’ve heard my colleagues complaining about how it’s not like the “good old days.” They would tell my son not to become a doctor. He didn’t heed that advice, and last week moved to Palo Alto to start an IBD research program at Stanford.
I prefer to look at the positive side. I love what I do and I’m good at it. I love my partners, who always want to help out. I love the hospital nursing and ancillary staff. They always seem happy to see me. I’m 74 years old but why would I retire? I’m having too much fun. Plus, every day there are at least one or two amazing patient stories that arise.
The practice of medicine will continue to change, for the good and bad. Accept the inevitable and learn to work with it. You will be much happier than if you fight it.
Mark Rosen, MD
mrosen@austinkidney.com

Submitted August, 2021
by Dr. Anna Vu-Wallace
No One Dies of COVID
“No one dies of COVID, right?” This was one of the first questions my patient asked me in our initial encounter. My immediate thought: “What??!!” He went on to say, “It’s just another virus, like the flu, I am told.” My response: “Who told you that? Where did you get your information?” Despite the calm exterior, I felt intensely angry. Unfortunately, I didn’t get to stay in anger long. Within hours, my patient was intubated. Even before he was intubated, he couldn’t believe he was heading into respiratory failure and needed a ventilator. The following days were struggles to keep his vitals and numbers stabilized. Some days we were successful, other days we were not. He died two weeks after his intubation.
I am certain many of my hospital colleagues encountered similar patients during these past 17 months. I heard sarcasm and anger from physicians and nurses, echoing my own internal attitude towards these patients. It had been building up to this point for me since the beginning of the pandemic. Like everyone, I had my fears when the pandemic started. In the beginning, there was so much support for those of us in the hospitals.
Then, it started to fade when misinformation surfaced. Anti-mask protestors appeared with subsequent bans on mask mandates. In a divided country, there was even more division on this point. The anti-vaccine movement seemed to end our patience the moment it started. I saw the outpouring of anger and disbelief from the medical community. By this time, it felt as if we were abandoned by the public. How can any of us not feel anger? We have every right to be. We are human, after all. Many have been overworked for years and were asked to give even more.
Staying in anger, disappointment, and negative emotions has had its effect. Fatigue and burnout settled in. Dr. Sarah Smiley, the leader of our hospital practice, defined the state as “…haggard and stressed,” in referring to all the nurses, therapists, doctors, chaplains, and hospital staff. “Even the greeters and security guards are weary,” she recalled.
My daily calls to families, much to my surprise, became a part of my healing. The personal calls led me to understand who my patients were and what led them to believe what they believed. These daily calls allowed me a look into the person, not the “annoying, ignorant patient” as judged by this physician, but a human whose life has been rich in gifts they gave to others. I realized, when I am in judgment, that it just takes knowing the other person, really knowing them, to understand and let go of judgment. I heard the sounds of their weeping and understood how much my patients’ lives touched those who knew them.
Dr. Elizabeth Kubler-Ross said, in so many words, to truly serve altruistically, we must understand our own biases and let them go before entering a patient’s room. These phone calls were often the only thing I could give to families to comfort them. The calls were often the pause I needed to look at my own biases and judgment, and just listen. Surprisingly, anger and frustration softened. My practice partner, Dr. Pamela Cowper, said recently, “I thought that I would have little sympathy for these patients who were not vaccinated, but I found it to be the exact opposite. I am rooting for them all. I am sure I picked the right career.”
The pause and listen seems to be key. False perspectives from my patients do arise from some element of truth. My husband, a retired business executive, life coach, and minister, reminded me, “To be open to another perspective, a person needs to first feel validated in some way that her/his own perspective has merit on some level, too.” Married to a highly educated and non-medical person, my husband also reminded me that despite his graduate studies, he knows nothing of the medical world. He said, “I don’t even know what questions to ask! I wouldn’t know who to believe if I didn’t marry a doctor. How would the public know who to trust given all the information out there?” This is a really good point. When I first met David, he didn’t know the difference between generic and brand name meds. He didn’t even know he could ask for generic medications, just as I would be clueless in his area of expertise.
So, how do I serve during such a tumultuous time? How do I serve those I disagree with? Pausing, listening, acknowledging other perspectives, and respecting the other person provided a space for conversation that can lead to change and healing. I don’t deny my emotions when they arise. I feel them and try to express them in a more constructive way. My anger and reactivity has not changed anyone. There is so much negativity now that I am careful not to add to it. I certainly don’t want to stay in negativity. It has not served me nor anyone else so far. By pausing and truly listening, I can reach for understanding. I am still working on this. It is an art after all….this doctoring.
Dr. Anna Vu-Wallace
annavuwallace@gmail.com

Submitted August 22, 2021
by Dr. Michelle Owens
I Don’t Want to be Resilient
I went to replace four hanging plants at a nursery this past weekend because they all died once the Texas heat made its appearance, despite being watered, placed in the shade and talked to by my daughter and me.
While I was looking for plants that will hopefully survive the Texas summer, I was chatting with my husband who cheekily said, “those plants weren’t resilient.”
He of course knows my disdain for the word “resilient.” I have shared quite a few times this year why it makes me cringe so much. The term “resilient” has been thrown around so flippantly since COVID that it is a real buzzword now.
As I have told my husband before, I do not want to be resilient. Being resilient to me means you’ve survived a dumpster fire white knuckling the whole way through at the brink of death but then manage to come out on the other side, traumatized, but still alive. Some might describe their experiences with COVID this way.
I believe there are ways we can be more proactive to fend off having to be too resilient too often.
I challenged him and said, “I do not want resilient flowers, I want hearty flowers. In fact, I want to be hearty.”
A quick Google search provided me the Webster Dictionary definition of the two:
Hearty means “vigorous and cheerful”; “strong and healthy”; “wholesome and substantial.”
Resilient means “able to withstand or recover quickly from difficult conditions.”
Looking at the image search is even more telling - hearty images show wholesome stews and soups, while resilient images show a human figure pushing a boulder up a hill.
I would much rather have a solid, hearty foundation than a resilient one marred with cracks, chips, and unevenness.
I worry that many organizations think “resilience training” is the answer, that if we all had a little more training in resilience, we would all be better for it. Honestly, I think resilience training is counterintuitive, exhausting and a slap in the face to the person having to complete it. Retroactive resilience training when staff are already burned out just contributes further to their burnout and feelings of failure.
The need to provide resilience training suggests that our perceived lack of resilience is the core problem, that “if only you were more resilient, you’d be happier/less burnout/ etc.” Perhaps we and our lack of resilience really isn’t the problem?
We all know watching a module on resilience, sitting in a lecture about mindfulness, being told to practice more yoga and breathing techniques does not make you feel less burnout. It’s having the support and buy-in from your workplace, to actually have the time to do the things that feed your soul and fill your cup. Adding more onto an already overflowing plate of life’s stressors only makes it heavier and more overwhelming.
I want support. I want authentic connection and compassion. I want someone invested in my well-being who prioritizes my self-care to prevent me from having to be perpetually resilient. I want someone who values my heartiness and helps to cultivate an environment that fosters continued growth for myself and others.
Dr. Michelle Owens
mowensdo@gmail.com

Submitted August 15, 2021
by Dr. Christopher Chenault
My Journey in Medicine and Life
I have been reading Dr. Sayers’ articles on the TCMS Wellness Program page as it provides a window into other lives in this journey of medicine and life in general. We all start out on a road that would seem quite like other travelers in training and practice, but we all find a unique and special way of stepping over or around the rocks and pebbles on the way. Some of us find these obstacles more difficult to ignore or put behind us, leading to more worries.
I do not wish to be too pollyannaish, but I have found medicine to have been a wonderful world in which to participate. Of course, medical school was a difficult goal to achieve, but when I finally got there it was exciting and challenging. We all knew it would be hard work and it lived up to its reputation. But it was grand and full of excitement and wonder. I scrubbed with Dr. DeBakey and Dr. Cooley and survived, held the artery after arteriograms, resuscitated a cardiac patient on the floor with only the respiratory therapist, delivered a lot of babies, set a few fractures, and did all the same things that all of you have accomplished and loved it. It was one of the highlights of my life. Following internship and general surgery residency, I spent two years in the Indian Health Service where I learned cert ain patient care techniques that I used the rest of my years in practice. My orthopedic residency was very much to my liking and they actually introduced me to the practice in Austin that I eventually joined. I found the group a remarkably congenial, smart, honest, and talented lot with which to practice. You just can’t find a better way to spend your days. Yes, we were in the ER a lot. One internist did the numbers and found that the general surgeons were called to Brackenridge about 110 times per month and the orthopedist around 103 per month. That’s a lot! But we had good dedicated colleagues with whom we shared that responsibility. Sure, sometimes in the middle of the night I felt a bit lonely and isolated, but I could call for help if needed.
During my practice, I realized you couldn’t run a school without a good PTA and you can’t run a hospital without committees. So, I served on a few committees where I got to know some doctors in other areas of medicine. The credential committee at Brackenridge and later at Seton brought some real insight into the workings of other departments and the complexities of privileging certain specialties. That also allowed me to get to know some of the staff and administrators in both the hospitals and the Medical Society. The talent observed lifted my days.
A wonderful wife and family took me on many unexpected journeys to a myriad of horse shows, band trips, uncounted band concerts, family travels, PTA live auctions, and all the crazy things that families do. The horror was losing one of our children that became the low point of our lives. With support of partners, family, friends, and our church we survived and moved on. You never completely move away from that but with support it becomes tolerable.
I don’t know why I feel so lucky because I know that many others are blessed as much or more than we have been. The comparison doesn’t make any difference. It is the absolute of what we live that is the joy. The opportunity to make at least a few people feel better in their pain makes the trip worthwhile. And the companionship of community is a remarkable balm to help manage the bumps in the road.
I present this story as a person who has very much enjoyed medicine as a vocation in spite of some complications and in contrast to the more difficult paths others have encountered.
And retirement is pretty nice also.
Christopher “Kit” Chenault, MD
cchenault@austin.rr.com

Submitted August 2021
Three Trout and Wisdom from the Ordinary
Let’s be honest about something that people are notoriously dishonest about. Fishing. I am just a terrible fisherman. I’m no good at picking bait. I’m impatient. I try to set the hook too early or too late. I can’t read the water in a Colorado stream nor see redfish swirling in the bay. Some years back I decided to take up flyfishing after re-reading A River Runs Through It, thinking I might fare better. On a magnificent stream in Colorado, I managed to catch two nice trout one memorable afternoon, but I’d have to say the day ended in a draw because I also hooked my fishing hat twice. I feel pretty sure that my father-in-law, a great outdoorsman, went to his grave wondering why in the world his daughter married such a terrible fisherman.
With our adult children and six grandchildren recently in Port Aransas, I was determined to catch some fish with my eight-year-old grandson. There was a lake behind the house, and we fished it some that first day, but all we managed to catch was a very unfortunate turtle. I gave in and hired a guide for some bay fishing, but when we got to the dock that morning there was a message that he had called in sick. You don’t tell an eight-year-old that a fishing trip is called off, so on advice from a local in the bait shop we went to a spot where we could fish from a pier or wade. What followed was at once predictable and surprising. He caught a croaker, just a bit bigger than what we could buy at the bait store, but as I was about to throw it back, he wanted to look at it. He marveled at the different colors that glistened in the sunlight, the spines, the pumping gills. Over the next hour or so we caught three small trout, none of them keepers, but he was amazed at how slippery they were and laughed as they repeatedly squirmed from his grasp when he tried to throw them back. By mid-morning nothing was biting, but several dolphins joined us just a few feet away much to his amazement, and in the end fishing that I would have called a dismal failure was a great time that he talked about for days. It was only one of many times that week when ordinary things − collecting shells, letting their feet sink into sand in the surf, feeding seagulls − things I hardly notice anymore, fascinated them, and through them, became visible again to me.
The evening before we left, I snuck out to the lake at dusk to try my luck again. It was a still evening, a full moon rising, and the lake was smooth as glass. John Buchan famously wrote, “The charm of fishing is that it is the pursuit of what is elusive but attainable, a perpetual series of occasions for hope,” a quote that fits even unsuccessful fishing well, and life in general. The casts were well placed, or so I thought, the results predictable but soothing nonetheless and I stood there in the quiet of early evening, Norman Maclean style, in the half-light where, however briefly, “all existence fades to being with my soul…and the hope that a fish will rise.” Perhaps there is more fisherman in me than I thought, seeing the essence of fishing before me, even without fish. I stood there and considered the lessons of that week: that there is wisdom in the ordinary, and with each cast, hope.
Brian S. Sayers, M.D.
PWP Chair
bsayers@austin.rr.com

Submitted, July 2021
by Dr. Michelle Owens
A Heavy Load
I want to share a short story from Jon Muth’s book “Zen Shorts” titled “A Heavy Load.” I’ve read it to my daughter and this particular story really spoke to me.
“Two traveling monks reached a town where there was a young woman waiting to step out of her sedan chair. The rains had made deep puddles and she couldn’t step across without spoiling her silken robes. She stood there, looking very cross and impatient. She was scolding her attendants. They had nowhere to place the packages they held for her, so they couldn’t help her across the puddle.
The younger monk noticed the woman, said nothing, and walked by. The older monk quickly picked her up and put her on his back, transported her across the water, and put her down on the other side. She didn’t thank the older monk; she just shoved him out of the way and departed.
As they continued on their way, the young monk was brooding and preoccupied. After several hours, unable to hold his silence, he spoke out. “That woman back there was very selfish and rude, but you picked her up on your back and carried her! Then, she didn’t even thank you!”
“I set the woman down hours ago,” the older monk replied. “Why are you still carrying her?”
How many of you also struggle with holding onto things that don’t bring you joy, but rather rob you of it?
Life is too short to hold onto things that weigh you down without any potential benefit in sight. I know I have struggled with this from time to time.
Our time and energy are invaluable; we need to be good stewards of it. Much easier said than done - I know. We are so much better at offering this advice to our families and patients rather than taking it to heart ourselves.
What’s one thing you can set down this week?
Michelle Owens, DO
mowensdo@gmail.com
Editor’s note: Our guest writer this week is Dr. Michelle Owens. Dr. Owens is a hospice and palliative medicine physician, wife, mom, native Austinite, self-care advocate, and current scholar in the AAFP Leading Physician Well-being Program.
Brian Sayers, MD
Chair, Physician Wellness Program
bsayers@austin.rr.com
Submitted July 2021
I can’t carry everything.
Knowing our limits is so important - they are critical in guiding us to set, respect and implement healthy boundaries, which in turn fosters our ability for adequate self-care. Asking for help is also crucial - and much easier said than done.
I am amazed at the self-care practices my 3-year-old daughter already has. She inspires me. She names her emotions better than most adults. She reminds my husband and I to “take a deep breath and calm our body,” and has healthier boundaries than I have ever had.
I’d like to think that some of the language she has acquired has been from me. I’ve heard myself say - especially as of late - I can’t do everything. I have found it to be a validating mantra and almost daily affirmation that I am not superwoman, I am not immortal and I am human.
She often times tells me this phrase, “ I can’t carry everything” at bedtime when she is trying to carry her baby doll and 2 unicorns upstairs. I always carry the 2 unicorns after she has asked for help; she always thanks me. We both feel better- her load is lighter and I’ve helped her. Win. Win.
I wanted to share this with y’all as a gentle reminder to know your limits, set healthy boundaries, don’t be afraid to ask for help and to give you hope for the future generations. ❤️
Dr. Michelle Owens
mowensdo@gmail.com
Submitted June 2021
Shame, Empathy, Connection,
and the Sinking of the Essex
I just finished a book about the sinking of the Essex, an early ninetieth century whaler that sailed out of Nantucket only to sink after being attacked repeatedly by a huge whale on the open sea. Only a few survived after three months at sea in small lifeboats enduring exposure, thirst and cannibalism, eventually rescued 3000 miles away off the coast of Chile. The captain survived and returned to Nantucket; the fantastic story of the whale attack confirmed but still suspect. He went to sea once more, his next ship hitting a coral reef and sinking. No longer employable as a captain he lived out his days in obscurity as a night watchman. Herman Melville, who wrote Moby Dick based on these events, met the beached captain and remarked, "To the islanders he was a nobody. To me, the most impressive man, tho' w holly unassuming, even humble…" As I finished the book, I could only think of the shame he must have endured, and I wondered if anyone cared.
A decade ago, I heard Brene’ Brown speak at my daughter’s high school. It was before I was familiar with her work and a toddler on the row behind me kept kicking my chair, but a line from her talk did stick and I’ve thought about many times since, especially in interactions with physicians experiencing distress or addictive behavior. I couldn’t recall the exact wording until I came across it recently: “Everyone has a story or a struggle that will break your heart. And, if we’re really paying attention, most people have a story that will bring us to our knees.” For the most part, those struggles, often involving shame, are mostly hidden from view, even when carried by people we think we know pretty well, smoldering and informing their behavior and mental well-being.
While guilt is a sense that “I did something bad,” shame is a sense that “I am bad,” and Brown describes it as “the swampland of the soul.” When shame is unaddressed it can cause despair that fuels destructive behavior, addiction and a variety of mental health issues. Brown points out that shame expresses itself differently in men and women. In men shame stems from the fear of being perceived as weak, in women of failing to live up to the complex web of expectations society lays on them. Beyond that, physicians in general are susceptible to shame, born of subtle indoctrination in training and early career to deny imperfections.
Brown notes that “empathy is the antidote to shame.” Like shame, empathy is a hot topic these days and has as many definitions as it does researchers. A basic definition would be “the ability to understand and share the feelings of another.” Author Sherry Turke’s slightly different view is that it means, “I have a commitment to be there for you. I don’t know how you feel, but I am here to listen.” Empathy requires connections, and while for some the pandemic strengthened our closest relationships, for others close connections with a network of friends and family normally available with empathy were lost or badly fragmented. Over time, this loss of empathetic connections has taken its toll on many, the dramatic rise in utilization of our counseling program and physicians leaving medicine only t wo of many indicators.
While empathy refers to our ability to take the perspective of, and feel the emotions of another person, compassion is when those feelings and thoughts include the desire to help. Compassion is the action that (hopefully) results from empathy. As a society of colleagues, we are meant to look out for each other. Actively. In ways that the institutions we inhabit can’t or won’t, we check in, we give space for the people we work with and care about to confide, to connect. Research has repeatedly shown that half of our colleagues are in distress from work, if not their life around it, yet we can’t fully appreciate it unless we are face to face with someone who is suffering, and take the time to recognize it. As Mother Teresa once said, “If I look at the mass, I will never act. If I look at the one, I will .”
Brian S. Sayers, MD
Chair, Physician Wellness Program
bsayers@austin.rr.com
Editor’s note: Our guest writer this week is Dr. Michelle Owens. Dr. Owens is a hospice and palliative medicine physician, wife, mom, native Austinite, self-care advocate, and current scholar in the AAFP Leading Physician Well-being Program.
Brian Sayers, MD
Chair, Physician Wellness Program
bsayers@austin.rr.com
Submitted, May 25, 2021
The Plight of the Family Rock
It only makes sense that as the doctor in the family, you would be the one that everyone goes to in times of crisis. I get it – it takes a certain type of person to persevere through all the challenges of medical education and training. But that doesn’t mean I have to like it. And that doesn’t mean I wouldn’t like to wish it away on more days than not.
The past 15 months have highlighted the plight of being the family rock. As if the global pandemic wasn’t enough to deal with, life goes on. Dealing with crisis and stress during normal times is hard, let alone having to juggle COVID-19 risk mitigation, social isolation and political extremes. So, this begs me to ask the question - Who is the rock for the family rock?
It’s exhausting to really sit down and think about it. And honestly, the best answer I can come up with is – a therapist. Paying someone to be your rock is one way to ensure you have someone to lean on when everyone else is leaning on you.
A wise mentor of mine during residency destigmatized the practice of seeing a therapist. She told me that therapy was part of her self-care. This makes so much sense to me now. I’ll admit that I was one of those people who thought seeing a therapist meant you were weak, imperfect (not an easy thing to swallow when we strive for perfection in the field of medicine), and there was something wrong with you.
Later I realized that no one is unbreakable or perfect. In fact, I would argue that those who see a therapist regularly are stronger than those who do not; largely due to the strength it takes to be vulnerable and share imperfections and perceived weaknesses.
Sadly, not all rocks become diamonds under pressure. Some become so damaged that they disappear. We can’t afford to lose any one of us. Consider lessening the burden with a therapist of your own – a good one is worth their weight in diamonds.
Dr. Michelle Owens

Submitted May 2021
The Winds that Brought Me Through
At first, I thought it was my imagination. Why are so many retiring, leaving medicine or “downsizing” their practice lately? A specialist with young children finally got fed up spending evenings and predawn hours keeping up with charting on too many patients and left fulltime practice to work part time and be more present with their family. A highly skilled specialist disillusioned with the system they worked in left medicine altogether. Seasoned colleagues still at the height of their skills with time to reflect during the pandemic decided that early retirement was not only possible, but imperative. An employed colleague whose hours and practice location were abruptly changed without adequate time to make childcare adjustments, left clinical practice. All took a financial hit which, in the end, paled in comparison to the emotional toll their work was causing. All at some point felt a sense of guilt in making the change, all felt betrayed that the demands or clash of values in their work left them no choice if they were to remain whole. It’s not just here. The sudden spike in doctors leaving medicine during the pandemic is a nationwide thing .
Heather Fork, who ran her own successful dermatology practice in Austin for almost a decade, knows as well as anyone what it’s like to discover her dream job was, in the end, not what she had anticipated. Although she enjoyed caring for her patients, she felt she wanted to help people in a different way and that the brief interactions with patients scheduled back-to-back was not an ideal way to have a meaningful impact. She closed her practice and, after a time of discernment in the Hill Country, became a Master Certified Coach and founded the Doctor’s Crossing, an organization that helps physicians re-examine their career path and explore options outside of clinical medicine. Heather’s already full client list has experienced a surge during the pandemic. To the usual reasons doctors consider leaving medicine, the pandemic added new ones born of the varied experiences doctors had that made us pause and re-examine our work. For some, it was a reduction in workload or more time with family that they are not willing to give up coming out of the pandemic. For others, it was the physical and emotional toll of working harder with suffering, death and safety issues a constant part of their work for months on end. For many, it became plain during furloughs, reassignments or other unwanted changes imposed by employers that they were undervalued and had little control over their work. Dr. Fork notes these and other factors “have the result of physicians feeling that they don’t really matter, except as RVU generators. They often feel unappreciated and expendable. This is not a good feeling for anyone, but when you’ve sacrificed many years of your life for this profession and then finally arrive and find out that your satisfaction is not important, it is very hard to continue sacrificing more of one’s life and well-being. Physicians are only human, and they too need what we all want, which is to feel valued, appreciated, and have freedom to serve in a way that brings joy and meaning.”
In the best of times, it can be challenging to fully connect with the joy and meaning that our work should bring to us, and these are not the best of times. Many of us are coming out of the pandemic knowing that change is needed in our work. Lately, for some that has meant “downsizing” schedules or changing practice settings entirely. For others, it means leaving direct patient care if not medicine altogether and, for our profession and our patients, that is tragic. Life is short and all moments within it are sacred, and we all deserve to be happy. We would all do well at this pivotal moment to re-examine life’s basic question posed by poet Mary Oliver:
Tell me, what is it you plan to do
with your one wild and precious life?
Most of us find great joy in our work, but for those who do not, there is a whole world out there waiting. Either way, we will always be colleagues.
While pretending to read journals the other night, a sappy movie about country singers in various stages of their careers was on in the background. It soon caught my interest because it had many parallels with medicine: passionate origins, early career enthusiasm, overwhelming time commitment, compromises with success, disillusionment, burnout. One of the songs had a line that reminded me of the colleagues I’ve had on my mind:
But I can’t do those things no more,
Like the way I’ve done before.
The same winds that brought me through,
Can blow that fadin’ flame out too.
Brian S. Sayers, MD
Chair, Physician Wellness Program
bsayers@austin.rr.com

Submitted April 2021
Regret
One of the surprises in the PWP counseling program has come from the anonymous questionnaires we ask colleagues accessing the program to fill out. To protect identity, we can’t ask much, but we do ask two questions − numerical assessments about satisfaction with work and relationships. It turns out that the responses are not very different from doctors who don’t access the program. But what I have found informally with physicians experiencing distress or dissatisfaction with work, relationships or life in general is a sense of regret, often involving a particular event or situation that triggers in them a call for change.
Regret feels bad because it comes with a sense of personal failure, is often visible to those around us, and is accompanied by self-blame, shame and sometimes guilt. Studies show that regret is a common emotion, 70% of adults having a significant sense of regret. While those studies demonstrate the most common sources of regret involve education, career, romance and parenting, I’ve found with physicians who seek support that their regrets involve relationships, career choices, medical mistakes, choices related to alcohol or substance abuse, or choices that adversely impact work-life integration. Researchers point out that regret related to inaction is more difficult to navigate than regret related to choices that turned out badly because the possibilities with the former are almost limitless as opposed to the more concrete consequences of the latter.
Regret can fester because left in isolation we often tend to dwell on it. As Amy Summerville describes “. . . we develop the reflex to chew and chew on an unfortunate turn of events, like a cow on its cud, till there is no nutrition left in it.” This can be paralyzing when major, life altering events occur that involve regret unless we reframe regret into something constructive.
All major religions and spiritual belief systems share a common theme that author Richard Rohr describes as the order→disorder→reorder cycle. Examples abound: traditional Native American cultures use metaphoric cycles of day-night-sunrise or the order of seasons, world mythologies consistently tell stories in a journey-fall-return to a new home pattern, recovery programs explore innocence-addiction-recovery, Christianity centers around life-death-resurrection. The list is endless but the point is the same: in any life, chances are we will at some point encounter what mystics called the “dark night of the soul,” a crossroads, with regret often a prominent feature, a place from which with some effort we might emerge into a new life that has not only escaped the bonds of regret, but has acquired wisdom from it. Rohr notes that even in distress we attempt to avoid the hard work of real change, the orderly progression from dis order to reorder and we often attempt to “jump from stage I to stage III,” of this common cycle, bypassing the personal growth that comes from confronting regret.
The liminal space between disorder and reorder is often described as a wilderness, a time of disorientation and unsure footing where the pathway out may be obscure. Discovery of that path is deeply personal and requires naming and confronting regret, openness and accepting support from family, friends, counselors, pastors, or a colleague, many of whom probably inhabited that same space at some point. It requires looking inward, self-compassion, a sense of hope and, perhaps the hardest part of all, patience. While in the wilderness, if we look closely, we may find angels that were sent to protect us, sometimes in the most unexpected places.
Author David Whyte sums it up well, “Sincere regret may in fact be a faculty for paying attention to the future, for sensing a new tide where we missed a previous one, for experiencing timelessness with a grandchild where we neglected a boy of our own. To regret fully is to appreciate how high the stakes are even in the average human life. Fully experienced, regret turns our eyes, attentive and alert to a future possibly lived better than our past.”
Brian S. Sayers, MD
Chair, Physician Wellness Program
bsayers@austin.rr.com
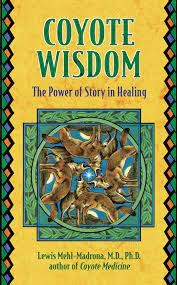
Submitted March 2021
Stealing Fire
Lewis Mehl-Madrona is a Native American physician who believes that nothing is more powerful in medicine than storytelling. It does not replace science or technology, but it shares an equal footing for those who truly practice the healing arts. Encouraging patients to tell the story of how their illness began in their own way and on their own terms can be a powerful tool in determining their path to healing. He notes that from a patient’s perspective, “Creation stories are also important because the final story about how you or I got well must be compatible with the story about how we got sick or the treatment will never work.”
Dr. Mehl-Madrona is the author of the “Coyote Trilogy.” He is a firm believer in the importance of the blending of what he describes as the bio-psycho-social-spiritual realms of illness in medical practice. His Native American roots inform him of the importance of the creation story, storytelling that is a crucial way of defining cultures, families, individuals, and even illnesses. “Stories contain and convey the meanings and values of our lives. They tell us how to perceive the world. They give us cultural identity . . . tell us about families and lives and what it means to belong. They comfort and heal us, both in the listening and the telling. They contain the living symbols we use to make sense of our world.”
Physician distress/moral injury/burnout that many physicians suffer in some ways is an illness of the soul and Mehl-Madrona's belief in the importance of exploring creation stories to make sense of illness applies as well here as anywhere else he describes it. Creation stories change with telling and retelling, evolves, matures, and becomes more interpretable, aided by those who help us through generous listening.
Hearing the story of others promotes healing for us as well as the storyteller. Particularly important is hearing stories of transformation, journeys from places of darkness into new life, a journey then envisioned by the listener. He notes that transformation is a logical evolution from closely explored creation stories as “Stories contain the hidden secrets of transformation, the alchemist’s formulas for turning lead into gold. If we hear enough stories about profound transformation, we find ourselves transforming, even in spite of ourselves. While we can’t command transformation, we can create an enriched environment that makes it more possible.”
While hearing a story can be healing, so too is telling our own story. “In some African cultures a woman healer tends the storytelling tree. Traumatized and suffering people come to the tree, place their hands upon it, and tell their story. Their suffering flows into the tree and away from them. Then they can walk away from that pain and trauma, because they have given it to the tree.” Telling our evolving creation story allows not only for an unburdening, but also helps us to make sense of the origins of things that trouble us, helps us understand the illness so that a path to healing can be envisioned.
Mehl-Madrona makes the point that in creation stories initial creation “leaves the people cold and unadorned. Within most cultures of North America, once created the people must steal fire to improve their lot−to keep them warm, cook their food, or give them light in the darkness. Fire is rarely just given to the people. It must be stolen or earned. Both Navajo and California natives steal fire. For the Cherokee it is given, but on top of a tall tree on an island far from shore with no obvious way to get it . . . The quest for fire also opens the door for heroic journeys towards new worlds of growth and development. Stealing fire arises from our dissatisfaction with the current state of affairs−stimulus to growth and change. Fire brings us light and warmth.”
There is little debate these days about the origins of physician distress. It is the result of difficult and often demoralizing systems that inherently caring and intelligent physicians are thrust into that has caused so much difficulty in our profession. We hope and work for change in these systems even as we do our best to function within them. In the meantime, we each have a creation story to tell about origins and the journey that brought us to the place we currently inhabit, for better or worse. Hidden within our creation story is the possibility of transformation. There is a story to be told. There is fire to steal.
Brian S. Sayers, MD
Chair, Physician Wellness Program
bsayers@austin.rr.com

Submitted February 2021
Broken Open
One of the things that defines families or lifelong friends is that while time and circumstance may cause us to drift apart, sudden tragedy or loss brings us back together, reminding us how important the connections with loved ones are, and how difficult it is to face life’s storms alone. In these last few weeks, we have witnessed our family of physicians in Austin figuratively, and often literally, reaching out to console, hug, encourage and commiserate over collective loss.
A friend who I share books with passed along Broken Open by Elizabeth Lesser recently. Lesser’s book is billed as an “inspiring guide to healing and growth…even in the face of loss and adversity.” I found myself less than fulfilled when I read the book, not that it doesn’t have profound truth in it, but rather that it seemed inadequate for the moment. In this and other times of unimaginable tragedy, people often, and rightly so, refer to the stages of grief, our search for meaning, the “hero’s journey” from mythology, the mystic’s “dark night of the soul,” scripture or other profound writings. All of these contain truth, even hope, but in the raw sadness of the moment when we feel lost, it can be difficult to find comfort or any grain of understanding in them.
These last few weeks, we have demonstrated, as colleagues with whom we have an unspoken bond of love and share much in common, how powerful it can be to come together as one, to support and be supported, to love and be loved, to remember and to look together for glimpses of comfort and hope.
A few years back, a patient of mine was telling me about a hobby of his, a passion really, called Kintsugi and I thought of him as I tried to make sense of these past few days. Kintsugi is a Japanese artistic practice and later a philosophy, with origins in the 15th century. Legend has it that the Shogun Ashikaga Yoshimasa always used his favorite bowl for the tea ceremony. The bowl was broken and sent back to China where a clumsy repair using a rusty staple was eventually returned to him. He instructed his Japanese craftsman to come up with a more aesthetic solution to repairing his cherished bowl and from that Kintsugi was born. In this practice, the tiny shards of a broken object are collected, sorted, cleaned and assembled one by one with meticulous precision. The pieces are precisely glued, then sanded, then the remaining cracks are filled in by successive layers of lacquer, then sprinkled with gold or other precious metal powder. The metal mingles with the moist lacquer to give an illusion of flowing metal. The gold “scars” are then burnished and a new work of art, meticulously created from the original, takes on new life. It is a practice that takes large measures of patience and time, for to rush the process leads to undesirable results rather than a thing of beauty.
The obvious metaphor from this is the basis of the Kintsugi philosophy of healing and hope. Even after profound damage, a healing of sorts may take place, but only over time, layer by layer, the shards of damage slowly pieced together, pieces slowly becoming part of the whole again. Though forever changed, it is eventually sealed and burnished, with patience and love, into an entirely new object, a lovely and precious piece of art that makes no attempts to hide its traumatic history, even as we marvel at its beauty.
Brian Sayers, MD
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com
Submitted January 2021
How to Save A Life
Once a year I’m asked to remind my colleagues about the work that the Physician Health and Rehabilitation Committee (PHRC) does and its availability to help our members. This time, as background, TCMS COO Belinda Clare gave me an article from 1989 written by Dr. Charles Felger about the work PHRC does. In the article, Dr. Felger notes, “We help our impaired colleagues not because we have to, but because it is the right thing to do…because we want to do so.”
For decades PHRC has been a source of support and structure to physicians in need, at any given time actively supporting 20-25 of our colleagues. Over the many decades of its existence, the Committee has helped hundreds rebuild their lives, be successful in their recovery, and safely continue caring for patients. Most of the physicians that we support are in recovery from alcohol or substance abuse and are monitored over a five-year period. Almost all are successful in their recovery, often against great odds. In my years serving on the Committee, I have seen many displays of courage and commitment from these brave physicians as they rebuild their lives and careers. On the day that we first meet with them, some of our colleagues’ very lives are at risk if profound change does not occur.
During a run recently I was listening to music and How to Save a Life came on. I had not heard it for several years and paid some attention to the lyrics. It was a well-known song a few years ago that describes someone trying to intervene with a loved one in crisis. The lyrics take us through a familiar scenario of how informal interventions tend to go when someone is brave enough to confront someone they love, with uncertain, and all too often unsuccessful, results. The refrain laments how inadequate we feel at times when we try to help someone in crisis:
“Where did I go wrong?
I lost a friend
Somewhere along in the bitterness
And I would have stayed up with you all night
Had I known how to save a life.”
In an interview with USA Today, The Fray lead singer Isaac Slade explained that the song is about an experience he had working at a camp for troubled youths: "One of the kids I was paired up with was a musician. Here I was, a protected suburbanite, and he was just 17 and had all these problems. And no one could write a manual on how to save him.”
We all feel inadequate at times like these, when someone we care about desperately needs help that they are not inclined to accept. It takes courage to confront, even intervene, in such situations, and initial attempts are often unsuccessful, but it is no less important to try. In my years on the committee, we have seen many people - friends, family or colleagues - courageously reach out to help someone, and as difficult as it is for all involved, the eventual outcome in helping our colleagues is almost always successful. The importance of taking the first step to help someone cannot be overemphasized.
How to save a life? As important as it is, the first step, to help someone (“Step one you say we need to talk…” the song notes) sets things in motion, but ultimately only one person can save a life, something we see, in awe, time and time again in the colleagues supported by the committee. We can set things in motion that might lead to recovery for people we love, but in the end, only they can save a life. Poet Mary Oliver describes it well:
But little by little,
…there was a new voice
which you slowly
recognized as your own,
that kept you company
as you strode deeper and deeper
into the world,
determined to do
the only thing you could do –
determined to save
the only life you could save
For more information about the committee contact Dr. Sayers at bsayers@austin.rr.com or Belinda Clare at bclare@tcms.com.

Submitted November 2020
The Knock at the Door
I recently read a piece by David Whyte that reminded me of an item on my long-neglected and largely imaginary bucket list, walking the Camino de Santiago, an ancient network of roads that lead to the shrine of St. James at a cathedral in Santiago, Spain. Christians through the centuries traveled these roads in pilgrimage, popular in modern times as a journey of personal growth or adventure. While the roads converge at the cathedral in Santiago, many “peregrinos” continue for a few more days to Finisterre, where the road ends at the ocean. Here, among several traditions, two are that pilgrims will burn something they carried on the journey, often a letter carried or written along the way, and also leave something behind that helped them to their destination, often their boots, both traditions highly symbolic and nowadays also highly discouraged by locals. Here, the pilgrim symbolically stands at the end of one journey, the beginning of another. Whyte writes of the experience in his poem Finisterre (abridged):
The road in the end taking the path the sun had taken,
into the western sea, and the moon rising behind you
as you stood where ground turned to ocean…
no way to make sense of a world that wouldn’t let you pass
except to call an end to the way you had come,
to take out each frayed letter you had brought
and light their illumined corners; and to read
them as they drifted on the western light;
to empty your bags; to sort this and to leave that…
and to abandon the shoes that had brought you here
right at the water’s edge, not because you had given up
but because now, you would find a different way to tread,
and because, through it all, part of you would still walk on,
no matter how, over the waves.
Whyte is writing about change at life’s biggest crossroads, and the sort of careful examination and courage that we are all called on to make at a handful of times in our lives when familiar paths we have followed need to be changed. We often feel paralyzed when change is needed, standing at the water’s edge as in the poem, trying to make that first step. 2020 has for many of our colleagues been a season of change, changes of both small adjustments, but also some larger ones that may change the trajectory of our lives well beyond the pandemic with our work, our families, our relationships. There are only a few things that really define our lives – faith, love, calling, hope, fidelity are some that come to mind, but so too is change, change that we have to consciously consider in one form or another through all the seasons of our lives to stay healthy, engaged, content.
Sharon Salzberg, author and advocate of Buddhist meditation, often uses the metaphor of a house where our soul lives. Visitors come to the door frequently, and we then decide how welcoming to be. Anger, fear, jealousy, doubt and shame are among the many visitors we may want to turn away, but instead, she recommends that we let them in and get to know them a bit. They are, unavoidably, familiar figures that come around often. The key is to get to know them a little, learn from them, then show them out. Don’t let them become residents or even overnight guests. Give them audience, then send them away. More often, invite into your home generosity, patience, gratitude, and love and encourage them to become more permanent guests in your house. In this metaphor, change will visit as well, the kind of change that we all need from time to time, a call to leave a familiar path behind for a new one, the kind of change you have to choose and have the courage to make. It may come to the door disguised in any number of ways, wanting not just an audience, but to become a part of your household at a time when its presence is needed, sometimes desperately. Whether we hear the knock, and how we respond, will make all the difference.
Brian Sayers, MD
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com

Submitted September 2020
Unleashed
I read an essay by poet Mary Oliver recently that describes her childhood home. Dogs roamed free until the town required leashing, and a dog catcher was hired. One particular dog, Sammy, was sort of a communal pet and did not take well to leashing. He showed up repeatedly in her yard, a chewed-through leash dragging behind him, unwilling to be tied. She eventually adopted him, and after appearing before a judge for being unable to keep the dog confined, she built a fence, which he promptly learned to climb. It’s a story about natural instincts to refuse unnatural constraints.
It made me think of medicine, through the ages, in recent decades and now in a pandemic. As a profession and as healers, we have been leashed in many ways over the years even as medical science and all of its miracles have emerged. One current restraint, a pandemic, is unique in its suddenness and completeness in so many ways, not just our work, but our lives in general. We have learned to recognize and respect that most of us have a certain uneasiness, or worse, that we often can’t quite put into words, and as skilled observers of the human condition we have come to recognize its effects on our patients and our colleagues, perhaps better than we recognize it in ourselves. Author David Kessler notes, “that discomfort you’re feeling is grief.” However we describe it, like familiar constraints imposed by the systems we work within, some aspects of it threaten to pull us away from what energizes us as physicians: a sense of meaning. As a good friend pointed out as I was writing this, too often we overlook the good things, the gifts, that we have received in the pandemic, and perhaps it is also a good time to acknowledge that some of the leashes we struggle with are self-imposed, bonds broken only through self-examination and, yes, resilience.
An article from several years ago asks the question, “What do doctors find meaningful in their work?” Studying narratives written by volunteers they found three recurring themes: a fundamental change in the doctor’s perspective, connection with patients, and making a difference in someone’s life. Change of perspective typically occurred after being part of a profound emotional experience shared with a patient. Connection with patients was described as occurring over hours or decades, involving moments of emotional intimacy, the doctor’s willingness to respond personally and genuinely, “being moved by their patient’s humanity…sharing their own emotions and life experiences.” Making a difference in someone’s life was not usually from brilliant diagnostic insight or skilled therapeutic intervention, rather it involved stories occurring in the setting of chronic, incurable illness, situations in which “doctors themselves were the principal therapeutic agents…awed that their mere presence could be healing and comforting to patients.” Common to each is recognition that sickness includes both disease, a disturbance of the body that needs our technical skills, and also illness, a disturbance of the soul that requires healing – humanity and connection – and therein lies the real meaning in our work. Each of these themes requires the physician to be undistracted and present in the moment, something difficult in most day to day practice settings. When we think about meaning in those terms, it is easy to see how so many things, lately the pandemic, may obscure recognition of moments that should energize us, make us better doctors, better human beings.
As for Mary Oliver’s Sammy, eventually, as he aged, he was harmless, but no more likely to allow himself to be confined, and the town turned a blind eye to his wanderings. The dog catcher who had rounded him up so many times quit, his career outlived by Sammy’s persistence. Unencumbered, she notes, “In this way, he lived a long and happy life…” Physicians through the ages, never more so than today, have looked for ways to break free of the leashes that distract, even separate us, from finding meaning in our work, too often unsuccessfully. But meaning is still there, at times hidden, waiting to be rediscovered. One day the pandemic will subside, this latest leash broken and we will hopefully find ourselves, with gratitude, in a new landscape, appreciating the return of things so easily lost, the lessons learned, unexpected gifts received, recognizing what Mary Oliver describes as “the wonderful things that may happen if you break the ropes that are holding you.”
Brian Sayers, MD
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com
Editor’s note:
Our guest blogger this month is Dr. Lauren Crawford. Dr. Crawford is a plastic surgeon and founder of Lady Docs of Austin, a Facebook community of female physicians with over 1100 members. She serves on the PWP Steering Committee.
Brian,
bsayers@austin.rr.com
Brian Sayers, MD
Chair, TCMS Physican Wellness Program

Submitted August 2020
Confessions of a Physician Mom
I confess. I’ve done my best. But, I chronically fail at this so called work-life balance.
I’m a plastic surgeon. I’m a mom of two. I sometimes function as a cook. I’m an occasionally lousy wife. I am not gifted at keeping plants alive.
I’ve read all about the elusive work-life balance. I think it’s like hunting unicorns for Type A folks like me.
But, over 10 years of private practice, I have gotten better.
I think it is a personal journey for any professional woman juggling a family. Physicians are unique in that a patient’s immediate care takes priority. When you are managing the health and surgical outcomes of numerous patients on a daily basis, you’ve set yourself up for some failures on the home front.
And, this causes stress. Especially for the women.
This is not a dig against the guys who are doing it all too (both doctor and domestic-duty dads). Women tend to shoulder more of the domestic work in these dual income households. In a way, the physician moms want it because we like the control. But, we take our domestic failures harder. The burdens haunt us more. We worry about our patients. We worry about our kids.
We are often the nanny hirers, grocery shoppers, meal planners, cake makers, summer camp organizers, school snack preppers, family event creators, appliance consumer report readers, and carpool mom texters. The multi-tasking wheel running hamster wild in our brains never stops. It even invades our dreams.
With every physician at risk for ‘burnout’ or ‘compassion fatigue,’ you can understand why the female doctors are particularly at risk.
I talked with a colleague before sitting down to write this. He has known me since I started practice here in Austin. He remarked that I seem really good, better than he has ever known me to be. I reflected on that. I think he is right.
What have I learned that has made my life better? I brainstormed and this is my laundry list.
1) I picked an excellent partner in life who supports (not always loves) what I do. We talk when I am overwhelmed. We figure out how to share the family work. He is the most important person, my best decision. Every physician mom needs an ultimate helper. A second wife isn’t typically a legal option. So, you need to find your critical support.
2) If you find good childcare, hang onto that person! Pay them well. Remember every birthday and treat them well. That trust is ultimate peace of mind. Outsource and hire out what you need to survive as you can afford to do so. Please.
3) Be selfish and surround yourself with supporters. And, support them right back. Those carpools have saved me. I want to kiss the last neighbor mom who made us dinner. There are amazing helpers in your community. Find them.
4) Be honest and realistic with yourself. Don’t over plan weekends. Don’t create unlikely timelines. Overestimate the time you need to prep for that Saturday soccer game. Always feeling behind or late at both work and home is stress you don’t need.
5) Figure out what you need to SLOW THINGS DOWN. You’ve got to carve out some time for your thing. Whatever that is. You need to have consistent time carved out. For me, it’s what we call my ‘moving meditation’. Actual meditation is not my thing. Running is. My husband sees the antsy energy when it’s overdue. Adjust something in your schedule to allow a change of focus. You need it.
6) Let go of total perfectionism. Perfectionism plagues our profession. The biology of the human body does not allow for it. You’ll do better as a quasi-perfectionist. Keep the big picture, broaden your perspective, and ask yourself what really matters?
7) Relieve yourself of perpetual mom guilt. Your kids will survive an afternoon or a week of too much screen time. That laceration on the forehead will scar just fine. Eventually, your kid will not need a nighttime diaper. That dental appointment is only 3 months late. Relax! Truly.
8) Find your peer group and bounce your parenting, business ideas, grief, and concerns off on those trusted colleagues. Don’t go friendless because you are too busy. Everyone has some time to fire off a few text messages every week. Don’t let those relationships go completely dormant. Even introverts need people. Social media can have some benefits here for quick feedback from minds you trust.
9) Learn how to say no at work when it’s needed. It is a bit cliché, but people will abuse a doctor who is too available. When something is a poor use of your time, recognize it, and say no. But, also, choose your battles. A small detail in your office policy that doesn’t affect patient care may not be your hill to die on. Frequent conflict in the office setting is draining. If your work culture is bad, not fixable, and not sustainable for you, start your hunt for a new job. Be confident in your value. Invest in your happiness. Be willing to move for it.
10) To piggyback off of 9, it’s not a failure to leave a position that won’t work for you long term. You will be wiser as you research your career move and look for the things you and your family need.
I can’t overemphasize enough that I’m not a finished product. I think I’ll always be a work in progress. I’ve repeated some of the same old behaviors that have made me unhappy in the past with work. But, it seems experience and age has led me to doom myself less.
I look at my kids’ faces every night with no small electronic or work distraction. I just sit with them. We might be reading or watching a movie. Maybe a back scratch or drawing my fingers down the ski slope of their noses. Nothing big. We have some of our best conversations in those moments. And, it might just be for five minutes. But, it never fails to quiet my brain and make me feel happy.
I am so sorry for all the doctors out there dealing with additional stress in this time of COVID-19. You may have a sick family member (COVID or not). You may be worried about losing your job or you’ve already lost it. Much love to you all as you navigate this tremendously difficult time as physicians.
Lauren Crawford, MD
Submitted July 2020
Editors note:
Our guest writer this month is Dr. Anna Vu-Wallace. Anna is a Hospitalist, PWP Committee member and Director of the quarterly Stress Reduction Meditation Workshop for Healthcare Professionals.
Brian
bsayers@austin.rr.com

Dear Friends,
Being in the hospital gives me a unique perspective on the current situation of the pandemic. Some of you shared with me that you don’t even look at the news anymore. That is understandable given the tumultuous period of our time. There are other ways to obtain vital information. This is a link to our statistics on COVID locally.
As hospital physicians, we are tasked with reaching everyone who may have influence as we see the sharp rise in our county and state. As I write you today, our hospitals are filling up. We are near capacity as we prepare our convention center for overflow.
Let me share with you what my typical day looks like. Shortly after awakening, I put on my scrubs and head out. Fear of taking this virus home and infecting my family takes hold as I don my N95 mask tightly to my face. Protective goggles are placed. Shoes from the day before left in the garage wait for me to put back on. As I enter the hospital, another mask is placed on me along with a shield. As I enter the COVID unit, I am covered with a gown and hair cover and 2 layers of gloves. My shoes are covered with shoe coverings. By the end of the first hour, my face and ears are painful due to the gear I must wear. The back of my ears bleed on occasion. By the time I get home, indentations mark how long I have been working. I strip off my contaminated clothes in the garage. I dare not to touch anything until I shower. Even then, I know how unpredictable this virus is. I pray my family will be ok as I have decided not to find different living arrangements isolating from them as there is no end in sight.
I attend to many. Without a definitive treatment for COVID, the sorrow of families of the dying is often overwhelming, relentless.
Today, I learned that at least 12 nurses I worked with have been infected and sick, 7 hospitalized. There have been at least 4 physicians infected. I know some will die. Our nurses are at the greatest risk. The longer we are exposed to COVID-19, the higher our chances of getting infected and sick despite PPEs. We are seeing such a steep climb in hospitalizations that Travis County becomes a topic of national news each night. What can I do? I can ask for your help. Would you make your own plea to your patients, friends, and family? These are some of the things we ask to help us control the spread of COVID-19:
-Would you wash your hands frequently, wear a mask outside of your home and physical distance for the next year?
-Would you not invite friends to come to your home for dinner/drinks until our local health departments clear to do so?
-Would you stay home when possible? We have a stay home order from Mayor Adler.
-Would you hold off on any church gatherings until we see a trend downwards for at least 2 weeks?
I know this is difficult. Community is vital to our very human journey. From my perspective, we are still in community, just in a different way. In our difficulties, there is an opportunity for growth. We can now see disparities in access to healthcare and what populations are at greatest risk. We can now see how our system is broken and can work for change.
Before sending this email, I explored my motivation. Yes, I don’t deny that I ask for me. However, I also believe I ask for all of us. What I have truly learned from this virus is how connected we all are. What we do individually will affect the collective.
In gratitude,
Anna Vu-Wallace, MD
Submitted
June 2020
Wabi-Sabi

Like many
of you, I’ve spent the last few months on a new and unpredictable schedule.
Doing telemedicine from home (where I never seem to have quite what I need),
then back to the office to see folks that need to be seen in person,
semi-hypoxic from masking, with schedules, workstations, basic procedures all far
from the routines and systems I’ve arranged in my office all these years. In
medicine, if not life in general for some of us, there is an unspoken quest for
perfection. Perfection that provides the kind of care for patients that we want
for them, perfection that might isolate us from criticism, perfection that
makes our days flow seamlessly. Of course, we know that imperfection and its
twin, uncertainty, is actually what punctuates our days, and how we navigate
that has much to do with our happiness. I’ve found that patients have generally
been flexible and understanding about the new level of imperfection and
inconvenience in medical care these days, certainly more so than me. Navigating
those challenges has even formed a new kind of bond with some of my patients
who have needed more help lately, and relaxing a bit and accepting imperfection
and uncertainty might, perhaps, produce a new kind of wholeness described in
this way by Rachel Remen:
“The
marks life leaves on everything it touches transforms perfection into
wholeness. Older, wiser cultures choose to claim this wholeness in the things
that they create. In Japan, Zen gardeners purposefully leave a fat dandelion in
the midst of the exquisite, ritually precise patterns of the meditation garden.
In Iran, even the most skilled rug weavers include an intentional error, the
“Persian Flaw,” in the magnificence of a Tabriz carpet. In Puritan America,
master quilt makers deliberately left a drop of their own blood on every quilt
they made; and Native Americans wove a broken bead, the “spirit bead,” into
every beaded masterpiece. Nothing that has a soul is perfect. When life weaves
a spirit bead into your very fabric, you may stumble upon a wholeness greater
than you had dreamed possible before...”
In traditional
Japanese culture, wabi-sabi is a world view centered on the acceptance of the
transience and imperfections of life, the natural cycles of growth, decay and
death, the beauty of nature, the frayed edges of existence. Derived from
Buddhist teachings, it stresses simplicity, humility, intimacy, and
appreciation of the natural world. Control, possessions, and predictability are
notably absent. Our lives in the time of coronavirus, and beyond, are marked by
existing in a magnificent but imperfect world in which we all live imperfect
lives, creating a kind of kinship with all humanity. From impermanence and
imperfection may come frustration, anxiety, and sadness, but also the
possibility that we might find growth and acceptance, see the world through a different
lens, even discover self-compassion, the very definitions of wisdom that comes
to us only through living in harmony with the imperfections of life.
Brian Sayers, MD
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com
Submitted May 2020
Telemedicine and the Opening of Eyes

Like many of you, a very short time ago I made the transition to telemedicine visits almost overnight, just as countless other changes went on within our small practice. While imperfect, telemedicine visits in the current environment offer a certain kind of safety that we just can’t pass up. I knew that there would be significant disadvantages, but I would soon learn that this strange new world of sitting in my study and suddenly finding myself inside of my patients’ homes might add an entirely new dimension to my relationship with them.
Even the simple platform that we use presents significant hurdles for many of our older patients, and our receptionist, now repurposed as our “IT Hostess,” sometimes spends more time getting them online and their mic and camera working than I do with the visit. The first week I’ll have to admit I was entirely distracted by the patients’ surroundings. Most use a laptop set below their face and I am often greeted with a perfect anatomic tour of their nostrils and popcorn ceiling. For those who position the camera at eye level, there is invariably a background nothing short of fascinating, even when entirely ordinary. On the wall behind them I have seen everything from 50 year old wedding pictures to an image of Jesus, family photos, and on memorable occasions a Grateful Dead concert poster, part of what I think was a framed rendering of “dogs playing poker,” and once, what appeared to be a varmint tail of some sort nailed to the wall. I’ve seen kitchens in the background with a concerning array of dirty dishes, but also palatial surroundings, breathtaking hill country or lake views and magnificent art. Occasionally, when the name of a certain medicine eludes them, I get a walking tour of their bathroom and medicine cabinet.
The initial fascination with my patients’ surroundings soon gave way to what it should have been for me all along: a sense of appreciation to see them in their natural surroundings, generously inviting me in. More often than not they are chatty, often much more interested in having some company in for a visit than telling me much about their medical issues. I have come to see that in these visits, if I take some time, I learn more about them and who they are than I have in 20 years or more of in-office visits. Invited into their homes, I have been given a seat on what to them is sacred ground, and with most I feel a new sense of kinship, and witness a certain vulnerability and hospitality that must have been what caused our predecessors to keep doing house calls with little complaint until not so long ago. On a good day, when I allow it, telemedicine visits help me to see my work and my patients through new eyes. Perhaps this is what physician wellness pioneer Rachel Remen had in mind when she penned these words:
“Often finding meaning is not about doing things differently; it is about seeing familiar things in new ways. When we find new eyes, the unsuspected blessing in work we have done for many years may take us completely by surprise. We can see life in many ways: with the eye, with the mind, with the intuition. But perhaps it is only by those who speak the language of meaning, who have remembered how to see with the heart, that life is ever known or served.”
Brian Sayers, MD
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com
Submitted April 17, 2020
The Upside of Uncertainty

There is not much in our lives that hasn’t changed drastically in the last three months. Each of us is experiencing fallout from the pandemic in our own unique way. Each of us is writing a story that will only be fully told months or years from now when we see these events with the perspective that only time can give--hopefully from a place of relative safety, a place where it may seem like we have all collectively exhaled. Our lives are not just drastically different at this time but will just as certainly never be the same, in ways that we are only now starting to see an outline of. There is great tragedy, danger, fear and anxiety all around us, a sudden uncertainty that is at once disturbing and disorienting. But just as surely, there is emerging an unexpected upside from this time of uncertainty.
This past week, I asked members of the Physician Wellness Program Steering Committee to write a few lines for me regarding strategies and observations they have to offer during this difficult time. By far the recurring theme was that this communal “time out” of sorts has, even with stress and tragedy around us, brought us closer together as families, helped us appreciate our friends and colleagues and our work, all of which we so often take for granted. It has caused most of us to pause some work activities, volunteer commitments, our children’s overextended schedules, the frenzied pace of our lives. While some of us are busier than ever dealing with the fallout of the pandemic, many find themselves on a reduced schedule, certainly at home more, and with other commitments lessened, time to think, to reassess priorities, schedules, friendships and family. Time to realize how much we assume, how little we reflect, how much we miss. Several observed that this time of uncertainty has bred a new sort of gratitude and compassion and feel that it may just give them a second chance to bring about positive changes in lifestyle and outlook.
More of the Committee’s observations and strategies for weathering the storm, along with notes about recently enhanced PWP programs on this video.

Physician Wellness Counseling
- Featuring our outstanding psychologists
- Remote/telemedicine visits
- Psychiatry volunteers
The Physician Wellness Program offers anonymous, free sessions with TCMS vetted psychologists. So far, the program has funded over 500 confidential sessions with our therapists.
As an added benefit of the program, for the next three months, TCMS has a referral list of psychiatrists who have offered to participate in the program. If you feel you would benefit from seeing a psychiatrist in addition to, or instead of, a psychologist, let us know when you call the helpline.
The program can be easily accessed, and privacy is strictly protected. A certified Gottman Couples Therapist is now available in addition to individual counselors to help with work, personal, or marital issues.
The cost of the first four sessions is covered by the program.
Whatever the issue, this program is your safe harbor. Nothing is reported, no diagnosis made, no insurance billed.
To access the program, call the wellness line at 512-467-5165 or visit the PWP counselor page.
Submitted March 20, 2020
Confidential, free counseling program for TCMS members and spouses now offering telemedicine/remote services.

Masks, gloves, raw hands, empty store shelves, telemedicine, nosediving stock market, the very real concerns for our loved ones and ourselves. Uncertainty. Chaos. Yet in the midst of it all, our TCMS members are doing amazing things for our community. But for some, it comes at a price.
For the past two years the PWP Counseling Program has been there offering convenient, anonymous, free counseling services by our vetted doctorate level therapists. Over 500 visits have been sponsored by the program to date.
To make things even more accessible in these stress filled times, all five of our therapists offer initial visits by phone and are now offering ongoing counseling via telemedicine in the privacy of your home, office or where ever you want to access it.
Take a minute to check out your medical society’s PWP program and our therapists’ bios. Call our anonymous Helpline 512-467-5165 for assistance, or contact one of our therapists directly . Just identify yourself as a TCMS member (or spouse) and they will take it from there.
Stay safe. Stay connected.
Brian Sayers, MD
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com
Submitted March, 2020
Profiles in Courage

A recent story I read about Washington politics made reference to John Kennedy’s Pulitzer Prize winning book, Profiles in Courage. Kennedy wrote the book while still a senator, a book that looked at politicians who had, at their own personal or political peril, taken courageous moral stands that were counter to party or popular opinion. I spent some time with it, hoping to see a model that might help me recognize admirable courage in modern day Washington. There is a quote in the introduction that caught my eye. “To be courageous . . . is an opportunity that sooner or later is presented to us all . . . in whatever arena of life one may meet the challenge of courage . . . each man must look into his own soul.” I gave up considering where courage might or might not be in Washington as thoughts turned to who closer to home I’d consider courageous. I did not have to think for long.
For almost a decade, I’ve served on and chaired the TCMS Physician Health and Rehabilitation Committee. PHRC advocates and assists in monitoring our colleagues who are in recovery from alcohol or drugs, its goal being to help physicians in whatever ways we can to be successful in their recovery, to protect their license and livelihood, and to see them on a path to a new and fulfilling life. The committee is made up of physicians from all kinds of practice settings and specialties, including psychiatrists and addictionologists, active and retired, some in recovery, others simply interested in helping their colleagues. My own path was as an adult child of an alcoholic, a father who died of alcoholic liver disease at age 40 as the 12 year old version of me looked on, in an era when getting help was greatly stigmatized. For recovery to be successful takes great personal courage. It also takes the help of others.
In a recent interview, Elton John made reference to the importance of community, of asking others for help, in the process of recovery. “We were all people who had made bad choices and seen the consequences, but then made the same choices despite ourselves . . . again and again and again. The truth of it all was that simple: no matter where we had come from, what we had accomplished or failed to accomplish, what our life experiences had been up to that point, we were all the same. And none of us would get better without asking others for help.” And so it is that PHRC exists, to play at least a small role in helping those in recovery.
Our colleagues who go through our five-year monitoring program all have their own story, unique origins that brought them to us, but there is a common pattern. There is usually anger and denial early on. After an extended stay in rehab which most of them agree to and are successful with, they reemerge with less anger and denial, often replaced by a period of a sort of disequilibrium, even as they see the framework of a new future emerge, as they lean into the gale force winds of early recovery. As we get to know them better over time, I invariably see a kind of raw courage and determination, mixed with a new sense of humility and vulnerability that does indeed propel them into a future of hope, often a new appreciation for things lost and regained, and a rediscovery of sacred worthiness that was there all along, but hidden. By the time their five years with us are completed, I think we usually consider ourselves to be friends, and I consider myself lucky to know these men and women of courage as they leave the program and as I have a chance to see them beyond the walls of the committee room.
Our work as physicians can be rewarding, bring great satisfaction, even joy, but it can also be frustrating and stressful, sometimes causing us to question our calling. Doctors are humans and humans are fallible, capable of terrible missteps that can alter not only our own lives but also those around us that we care for. As I’m writing this piece, I have been reading a book by Gregory Boyle, Tattoos on the Heart. In it he closes one chapter with a memorable line worth considering as we do the sometimes difficult work of caring for each other: “Just assume that the answer to every question is compassion.”
Brian Sayers, MD
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com
Submitted February, 2020
Beyond Burnout: Docs Decry Moral Injury From Financial Pressures of Health Care
By Melissa Bailey

Dr. Keith Corl was working in a Las Vegas emergency room when a patient arrived with chest pain. The patient, wearing his street clothes, had a two-minute exam in the triage area with a doctor, who ordered an X-ray and several other tests. But later, in the treatment area, when Corl met the man and lifted his shirt, it was clear the patient had shingles. Corl didn’t need any tests to diagnose the viral infection that causes a rash and searing pain.
All those tests? They turned out to be unnecessary and left the patient with over $1,000 in extra charges.
The excessive testing, Corl said, stemmed from a model of emergency care that forces doctors to practice “fast and loose medicine.” Patients get a battery of tests before a doctor even has time to hear their story or give them a proper exam.
“We’re just shotgunning,” Corl said.
The shingles case is one of hundreds of examples that have led to his exasperation and burnout with emergency medicine. What’s driving the burnout, he argued, is something deeper — a sense of “moral injury.”
Corl, a 42-year-old assistant professor of medicine at Brown University, is among a growing number of physicians, nurses, social workers and other clinicians who are using the phrase “moral injury” to describe their inner struggles at work.
The term comes from war: It was first used to explain why military veterans were not responding to standard treatment for post-traumatic stress disorder. Moral injury, as defined by researchers from veterans hospitals, refers to the emotional, physical and spiritual harm people feel after “perpetrating, failing to prevent, or bearing witness to acts that transgress deeply held moral beliefs and expectations.”
Drs. Wendy Dean and Simon Talbot, a psychiatrist and a surgeon, were the first to apply the term to health care. Both wrestled with symptoms of burnout themselves. They concluded that “moral injury” better described the root cause of their anguish: They knew how best to care for their patients but were blocked from doing so by systemic barriers related to the business side of health care.
That idea resonates with clinicians across the country: Since they penned an op-ed in Stat in 2018, Dean and Talbot have been flooded with emails, comments, calls and invitations to speak on the topic.
Burnout has long been identified as a major problem facing medicine: 4 in 10 physicians report feelings of burnout, according to a 2019 Medscape report. And the physician suicide rate is more than double that of the general population.
Dean said she and Talbot have given two dozen talks on moral injury. “The response from each place has been consistent and surprising: ‘This is the language we’ve been looking for for the last 20 years.'”
Dean said that response has come from clinicians across disciplines, who wrestle with what they consider barriers to quality care: insurance preauthorization, trouble making patient referrals, endless clicking on electronic health records.
Those barriers can be particularly intense in emergency medicine.
Corl said he has been especially frustrated by a model of emergency medicine called “provider-in-triage.” It aims to improve efficiency but, he said, prioritizes speed at the cost of quality care. In this system, a patient who shows up to an ER is seen by a doctor in a triage area for a rapid exam lasting less than two minutes. In theory, a doctor in triage can more quickly identify patients’ ailments and get a head start on solving them. The patient is usually wearing street clothes and sitting in a chair.
These brief encounters may be good for business: They reduce the “door to doc” time — how long it takes to see a doctor — that hospitals sometimes boast about on billboards and websites. They enable hospitals to charge a facility fee much earlier, the minute a patient sees a doctor. And they reduce the number of people who leave the ER without “being seen,” which is another quality measure.
But “the real priority is speed and money and not our patients’ care,” Corl said. “That makes it tough for doctors who know they could be doing better for their patients.”
Dean said people often frame burnout as a personal failing. Doctors get the message: “If you did more yoga, if you ate more salmon salad, if you went for a longer run, it would help.” But, she argued, burnout is a symptom of deeper systemic problems beyond clinicians’ control.
Emergency physician Dr. Angela Jarman sees similar challenges in California, including ER overcrowding and bureaucratic hurdles to discharging patients. As a result, she said, she must treat patients in the hallways, with noise, bright lights and a lack of privacy — a recipe for hospital-acquired delirium.
“Hallway medicine is such a [big] part of emergency medicine these days,” said Jarman, 35, an assistant professor of emergency medicine at UC-Davis. Patients are “literally stuck in the hallway. Everyone’s walking by. I know it must be embarrassing and dehumanizing.”
For example, when an older patient breaks an arm and cannot be released to their own care at home, they may stay in the ER for days as they await evaluation from a physical therapist and approval to transfer to rehab or a nursing home, she said. Meanwhile, the patient gets bumped into a bed in the hallway to make room for new patients who keep streaming in the door.Being responsible for discharging patients who are stuck in the hallway is “so frustrating,” Jarman said. “That’s not what I’m good at. That’s not what I’m trained to do.”
Jarman said many emergency physicians she knows work part time to curtail burnout.
“I love emergency medicine, but a lot of what we do these days is not emergency medicine,” she said. “I definitely don’t think I’ll make it 30 years.”
Also at UC-Davis, Dr. Nick Sawyer, an assistant professor of emergency medicine, has been working with medical students to analyze systemic problems. Among those they’ve identified: patients stuck in the ER for up to 1,000 hours while awaiting transfer to a psychiatric facility; patients who are not initially suicidal, but become suicidal while awaiting mental health care; patients who rely on the ER for primary care.
Sawyer, 38, said he has suffered moral injury from treating patients like this one: A Latina had a large kidney stone and a “huge amount of pain” but could not get surgery because the stone was not infected and therefore her case wasn’t deemed an “emergency” by her insurance plan.
“The health system is not set up to help patients. It’s set up to make money,” he said.
The best way to approach this problem, he said, is to help future generations of doctors understand “how decisions made at the systems level impact how we care about patients” — so they can “stand up for what’s right.”
Whether these experiences amount to moral injury is open for discussion. Cynda Rushton, a nurse and professor of clinical ethics at Johns Hopkins University, who has studied the related notion of “moral distress” for 25 years, said there isn’t a base of research, as there is for moral distress, to measure moral injury among clinicians.
But “what both of these terms signify,” Rushton said, “is a sense of suffering that clinicians are experiencing in their roles now, in ways that they haven’t in the past.”
Dean grew interested in moral injury from personal experience: After a decade of treating patients as a psychiatrist, she stopped because of financial pressures. She said she wanted to treat her patients in longer visits, offering both psychotherapy and medication management, but that became more difficult. Insurers would rather pay her for only a 15-minute session to manage medications and let a lower-paid therapist handle the therapy.
Dean and Talbot created a nonprofit advocacy group called Moral Injury of Healthcare, which promotes public awareness and aims to bring clinicians together to discuss the topic.
Their work is attracting praise from a range of clinicians:
In Cumberland County, Pennsylvania, Mary Franco, who is now 65, retired early from her job as a nurse practitioner after a large corporation bought out the private practice she worked in. She said she saw “a dramatic shift” in the culture there, where “revenue became all-important.” The company cut in half the time for each patient’s annual exam, she said, down to 20 minutes. She spent much of that time clicking through electronic health records, she said, instead of looking the patient in the face. “I felt I short-shrifted them.”
In southern Maine, social worker Jamie Leavitt said moral injury led her to take a mental health break from work last year. She said she loves social work, but “I couldn’t offer the care I wanted to because of time restrictions.” One of her tasks was to connect patients with mental health services, but because of insurance restrictions and a lack of quality care providers, she said, “often my job was impossible to do.”
In Chambersburg, Pennsylvania, Dr. Tate Kauffman left primary care for urgent care because he found himself spending half of each visit doing administrative tasks unrelated to a patient’s ailment — and spending nights and weekends slogging through paperwork required by insurers.
“There was a grieving process, leaving primary care,” he said. “It’s not that I don’t like the job. I don’t like what the job has become today.” Corl said he was so fed up with the provider-in-triage model of emergency medicine that he moved his ER clinical work to smaller, community hospitals that don’t use that method.
He said many people frame burnout as a character weakness, sending doctors messages like, “Gee, Keith, you’ve just got to try harder and soldier on.” But Corl said the term “moral injury” correctly identifies that the problem lies with the system.
“The system is flawed,” he said. “It’s grinding us. It’s grinding good docs and providers out of existence.”
This story was originally published on the Kaiser Health News website. Illustration by Maria Fabrizio for Kaiser Health News.
Brian Sayers, MD
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com
Submitted January, 2020
A River Runs Through It

During that last week of the year when I picture myself on a warm beach or by a fire in the mountains, I instead found myself, along with my loyal but somewhat annoyed staff, manually entering “Quality” and “Improvement Activities” data to satisfy my MIPS requirement to avoid Medicare penalties two years down the road. Many of you will have no idea what I am talking about, your practice managers and EMR silently taking care of this each year, but for those increasingly rare souls in small practices wary from hearing complaints about “pajama time” and the other struggles and cost of maintaining an EMR, that tedious time at the end of the year somehow seems worth it.
As I wondered if clinging to my paper charts is a reasonable strategy or if I’m just the proverbial old man hollering at kids to get off my lawn, I managed to waste even more time as I tried to find something that might explain “value based medicine” and how my time with MIPS is worth the effort. MACRA’s QPP (Quality Payment Program) is supposedly part of the pathway to value based medicine. There is, of course, nothing inherently wrong with the idea that being paid to keep people healthy is a better idea for society than primarily paying us to do things for people after they are sick. What I couldn’t get out of my mind was the repeated reference to “value.” Not surprisingly, the word “values” is never mentioned.
In fact, many argue that the very source of what is wrong with medicine, and more specifically with doctors, has everything to do with values, and not nearly as much to do with value. There are certain values that can be traced back to the origins of medicine, ideas like fidelity, compassion, competence, kindness, respect, and responsibility to name a few, that make us as a profession who we are. Many say that physician distress and burnout are the direct results of working in a system that provides little or no incentive, often even obstacles, to our honoring core values of our profession. This time of year when I am most acutely aware of distractions that distance us from honoring values sacred to our profession, I am reminded of a quote from Goethe: “Things which matter most must never be at the mercy of things that matter least.”
There is a river that connects physicians of antiquity to us in our own time, and beyond. The shores that the river endlessly passes are the ever changing shores of advancing science and evolving economics. Both surely change the façade of medicine in every age, and will continue to do so in ways we can scarcely imagine today. But the river itself carries with it certain timeless truths, values that are the same in any age, even if often hidden beneath rushing currents. The river burnishes and refines the stones in its bed, stones that carry messages that if not sought out and given homage, remain hidden at our own peril, words of timeless wisdom from our predecessors that we must both receive and pass on. My favorite line from a lifetime of reading is from Norman Maclean’s, A River Runs through It. It reminds me of being mindful of the heritage passed on through the lineage of medicine.
“Eventually, all things merge into one, and a river runs through it. The river was cut by the world’s great flood and runs over rocks from the basement of time. On some of the rocks are timeless raindrops. Under the rocks are the words and some of the words are theirs.”
Brian S. Sayers, MD
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com
Submitted, November 2019
The Man with a Gun

Tony (not his real name) was one of those patients who came to be a friend. I was his doctor for 11 years, guiding him through some very difficult times with lupus. He was a handyman, a fly fisherman, husband, father and a man of deep faith. His condition was difficult to control but he always offered a smile as he patiently and hopefully waded through a series of treatments through the years. I’m a terrible fisherman, neither of the two necessary traits (patience and reading the water) coming naturally to me, but it didn’t keep him from giving me flies that he had tied himself, even giving me a handmade bamboo fly rod that to this day sits in my study closet unused, but treasured.
One afternoon during a busy clinic my receptionist urgently pulled me out of an exam room exclaiming, “There’s a man in the waiting room with a gun and he wants to see you… He has some papers.” To this day I’m not sure who or what he was other than a messenger of misery. I suppose he was a constable, but all I remember is him handing me some papers and thinking how ginormous the gun in his holster was, reminding me of a foot long handgun that Mattie pulled out of a flour sack in True Grit, or the gun that a sneering Clint Eastwood/Dirty Harry pulled and pointed, challenging a criminal to try and resist, “Go ahead . . . make my day.”
I hadn’t seen Tony for a while and it turned out that he had been diagnosed and quickly passed away with an aggressive malignancy, which a plaintiff’s attorney seemed to think I should have suspected, even in the absence of signs or symptoms as of his last contact with me. This was the era before tort reform in Texas, an era where hardly anyone knew a single physician who had not been sued at least once. Now it was my turn.
If you haven’t been through it, it’s hard to understand the emotions you go through during malpractice litigation. In some ways it attacks the very core of who you are as a physician, an accusation that you are doing exactly the opposite of what you swore an oath to do and spent all of those years training to do well. As is often, but not always, the case there was a strong sense of injustice, as I knew I had really done nothing wrong. I was forbidden by counsel to discuss it with friends or colleagues, adding an unhealthy serving of isolation to a plate full of shame and anger. To complicate matters even more, I was simultaneously grieving a man who I considered a generous friend. After a year of silent anguish, second-guessing myself and being suspicious of patients I once felt at ease with, I was as unceremoniously dropped from the suit as I had frivolously been added in the first place. There was a tremendous, but profoundly incomplete, sense of relief. Now even two decades later I still recall those emotions clearly, even as I ironically still treasure the fly rod Tony gave me.
As physicians we are called on to be many things by patients, and by ourselves. Compassionate, competent, vigilant, intelligent, patient, available, perhaps even perfect. Litigation, deserved and undeserved, remains a constant threat lurking behind any mistake or just bad luck, but fortunately not as much as some years back. This extreme kind of judgment against us has to some extent been replaced by 100 smaller cuts that we face from criticism from patients or their families, online reviews, peer review, insurance authorization denials, peer to peer reviews, colleagues, employers, practice managers, and at times, most damaging of all, from ourselves. Some of these criticisms are well-deserved, even constructive, and are to be carefully considered as teaching moments, while others are simply based on bureaucracy, greed, frustration or just nastiness. All of them challenge our deep and ultimate calling to bring compassion and love, along with our talents, to each and every interaction with our patients.
Even Socrates noted 2500 years ago that “The unexamined life is not worth living” (though he was never “yelped”), so this is nothing new, though now it sometimes seems more personal, more public. Criticism is inevitable in our lives as physicians, as we are visibly out in the world doing things that matter, things that affect other peoples’ lives. Much has been given. Much is expected. We are not perfect. We were not designed to be. Along the way, people will surely assist us in realizing that.
Of course, we need to pay some attention to criticism, even when not kindly given. Criticism can be very valuable. Even when expressed inaccurately or with venom, there can be nuggets of truth. But there can also be a destructive element to undeserved criticism and judgment. We have to be careful, perhaps with self-reflection and support from our colleagues and loved ones, that this type of criticism does not harden us over time in a way that causes us to lose the compassionate calling that a younger version of ourselves set out to pursue all those years ago.
Brian S. Sayers, MD
Chair, TCMS Physician Wellness Program
bsayers@austin.rr.com
National Physician Suicide Awareness Day
Tuesday September 17
Submitted September 2019
Colleagues,
A few weeks ago we sent out a PWP blog, “My Friend Richard.” Many, if not most, of the PWP blogs sent out to 4000 or so TCMS members go mostly unnoticed. This particular one seemed to strike a nerve with some of you, and most who emailed me or stopped me in the hallway at the hospital afterward had a personal story of a friend or colleague who was lost to suicide, or came very close.
I don’t need to repeat the statistics that you have all heard so many times about physician suicide. I will just take the opportunity on this particular day to remind you to reach out for help if you need it. Once the honest and courageous decision to get help for the sake of yourself and those you love is made, help is readily accessible through family or a colleague or a friend you trust, or through our PWP Safe Harbor Counseling Program. And please, keep an eye out for your colleagues. If you sense they are in trouble, check in with them, say something. You just might be the person who makes all the difference for them.
Brian S. Sayers, MD
Chair, TCMS Physician Wellness Program
Check out this video
Submitted July 2019

My Friend Richard
There is something special about that childhood friend. It’s a bond that lasts a lifetime, something we can only experience fully in our formative years. My friend was Richard. We were inseparable in school growing up, then roommates in college, growing into manhood together. When it came time for medical school, I went to Dallas, Richard to Houston where he would start his career. We drifted apart in those years, each in a different world, each of those worlds with its own all-encompassing gravitational pull. I knew he had been depressed at times as far back as high school, but he always seemed to snap out of it. We took a vacation together on a break that last summer and he just wasn’t his old self. I couldn’t quite put my finger on what had changed but he was different. Our minds and energy were so preoccupied in that pivotal time as our careers were forming. A few months later I got the call one evening from a mutual friend in Houston that he had taken his life. As I tried unsuccessfully to piece it all together in the days, then years, that followed, there were fragmented stories of those last weeks, none fitting together. To this day I have no idea if he made any attempt to get help or if anyone tried to help him.
The current seismic movement in medicine to address physician burnout has its roots in a realization more than two decades ago that we were losing our colleagues to suicide at an alarming rate, much higher than the general population. In the last ten years there has been an explosion of research in this field, with a long overdue realization that the physician wellness crisis has little to do with the personalities we bring into medicine, and everything to do with the environment we are placed in from the day we enter medical school until the day we retire, or change occupation, or worse.
In the years since the TCMS Physician Wellness Program launched I have heard many stories from my colleagues about frustrations, loss of meaning, even stories of suicides in our community that I was unaware of. I have seen courageous colleagues get the help they needed with counseling or a recovery program, escaping a toxic work environment, cutting hours, developing healthier habits, connecting with colleagues, reconnecting with family or leaving direct patient care. Still, we find in some of our colleagues a certain sense of cynicism or anger or hopelessness, sometimes even a sense of shame that prevents them from getting help.
In a recent New York Times article, Clay Routledge writes about suicide as an existential crisis and notes that, “In order to keep existential anxiety at bay, we must find and maintain perceptions of our lives as meaningful.” He goes on to say, “How do we find meaning and purpose in our lives? There are many paths, but the psychological literature suggests that close relationships with other people are our greatest existential resource.”
The point is this. We all need to pay close attention to self-care in the many forms that must take. We need to get help from professionals and lean in to our family and trusted friends when we sense trouble and listen when those around us express concern. We also need to look out for each other. Check in with colleagues, especially if you sense they are struggling. What you think might be an awkward conversation with a friend might just save someone’s career, or their marriage, perhaps even their life.
My friend Richard may be the best friend I’ll ever have. I have many happy memories of growing up together, but also regrets. It is a difficult story even four decades later, but there is a happy ending of sorts, as his story, along with the stories of struggles of so many of our colleagues through the years, people you have seen in crisis, perhaps even your own story, are all embedded in this program and our growing desire as a community to be there for each other.
Brian S. Sayers, MD
Chair, TCMS Physician Wellness Program
Submitted June 18, 2019

Editorial Note: Our guest writer this month is Claire Miner, PhD, LPC. Dr. Miner is one of our PWP therapists, specializing in couples counseling. She can be accessed through our anonymous Physician Wellness Program coaching/counseling program by calling our confidential help line at 512-467-5165 or using the contact information at the end of her article.
CULTIVATING INTIMACY IN YOUR MARRIAGE
My friend is a gardener. Her flowers respond well to her care and attention. Some plants thrive with just a bit of water and sun, while others require fertilizing, a certain climate, and weeding to assure growth. In your “life garden,” you nurture your children and community with attention and resources. But is your marriage getting consistent “tending”? Even a healthy relationship will blossom with focused care. John Gottman’s Seven Principles for Making Marriage Work can point the way:
1. Enhance Your Understanding of Each Other
Know your partner and keep abreast of changes in his/her life. You know all the basic stuff, but do you know your partner’s inner world, such as his/her stresses, worries, aspirations, dreams?
2. Build Fondness and Admiration
Friendship is the foundation for passion and romance, and affection and respect are an important basis for friendship. Communicating the areas that you appreciate in each other will increase positive feelings.
3. Turn Towards Each Other
Everyday moments when people connect with each other are the building blocks of all relationships. “Turning toward” with emotional support, shared conversation and humor, exchange of interests, and affection will increase the positivity in the relationship.
4. Accept Influence from Your Partner
Being able to “yield to win” means that you won’t be a roadblock to change, and that you’ll be able to make your partner feel valued and respected. Focus on how to stay engaged and connected to your partner, rather than winning the argument.
5. Solve Your Solvable Problems
Couples in long-term, satisfying relationships have learned skills to solve the problems that can be solved in their relationship. These skills are not innate; we can all learn them—for example, starting a conversation gently and compromising.
6. Learn How to Talk about Perpetual Problems More Easily
Some issues between couples will never be resolved. The best that can be hoped for is to be able to find some humor in them and to be able to talk about them more gently and easily with acceptance, so that they are not great sources of pain.
7. Create a Vision for Yourselves as a Couple
One of the tasks of couplehood is to create shared meaning. Finding a vision to work towards together will enhance your sense of “we-ness” and keep you bonded as you move through time together.
Dr. Claire Usher Miner, PhD, LPC, Certified Gottman Couples Therapist, can be contacted at 512-689-7105.
Submitted May 10, 2019

Caduceus
Last month a couple of us from the medical society’s Physician Wellness Program spent a few days in Yellow Springs, Ohio at a training workshop conducted by physician wellness pioneer Rachel Remen, hoping to bring her well known Finding Meaning in Medicine small group program to TCMS. It was a transformative time spent with a collection of bright, motivated physicians mostly from prestigious institutions, who displayed exemplary humility even in the presence of a goofball like me. One of the group prompts was to bring a small object from our home or work that held some symbolic significance for our work. In one of the groups, someone had brought a small caduceus lapel pin given at medical school graduation. It reminded me of the power symbols can have, emotions they can trigger, stories or habits they can remind us of.
The caduceus is the classic symbol of our profession, its familiar gold staff, wings at the top and two serpents wound around it, tangled and climbing upward is actually different from the simpler, ancient version, the rod of Asclepius. A number of stories as to its meaning and origin exist. As Daniel Sulmasy recounts in A Balm for Gilead, the use of caduceus is derived from a story about Asclepius, the physician hero-god of Greek mythology from whom Hippocrates claimed lineage.
According to mythology, one day Asclepius was called to help a man who had been struck by lightning. While trying to save the man’s life, a snake came up beside him. Multitasking as physicians through the ages have, he quickly struck the serpent with a staff, killing it, then turned his attention back to his patient. Soon after another snake appeared, carrying herbs in its mouth which it promptly placed in the dead snake’s mouth. To the amazement of Asclepius, the dead snake was soon brought back to life. Taking the example, the mythological father of medicine took some of the herbs and placed them into the mouth of his own patient who was quickly healed.
Rich in symbolism, the story makes an important point about us as physicians and mortals. In classic literature the snake is often a symbol of our imperfections. Within that context, we see one serpent coming to the aid of another wounded serpent, then together climbing up the staff and away from their worldly moorings, healer and healed becoming as one, an image worth considering. We are instilled with a yearning to be like the winged staff, strong and reaching upward, but compelled to recognize that, like the serpents, we are vulnerable and in need of each other. It is the humility and response to this commonality, this broken oneness with all around us, that can make us healers in the best traditions of our profession, our ethics, our faith.
On the flight home, in that rare space where we might have a couple of hours to think, I considered again the trajectory of medicine in general and my own practice in particular. We all explore, in our own way, how we might become the kind of physician, the kind of healer, that occupied our dreams as our paths in medicine were being formed. Perhaps that will come from an ultimate realization that to be a great physician, rather than being the smartest person in the room, we need only be the kindest.
Brian S. Sayers, MD
Chair, TCMS Physician Wellness Program
Submitted March 25, 2019
Faith, Hope, and Transformational Leadership
I went back to school well into middle age and in class one day during a discussion on icons and Saints, the professor recommended that in the space where we work, relax or spend creative time, along with family photos we sprinkle in a picture or two of other people who somehow inspire us. It is a practice I had discovered years earlier and in my study are pictures of Abraham Lincoln and Johnny Unitas. The picture of Lincoln is just before his assassination in 1865, haggard and dramatically aging, but with a hint of a smile as the war came to an end. The picture of Johnny Unitas, the premier quarterback of his era and my childhood, is from the 1958 NFL championship game against the New York Giants, often called “the greatest game ever played.” It was the first nationally televised pro football game, a game that brought the NFL into the modern era. In the picture Unitas is raring back in classic drop back quarterback style to launch a ball far downfield that would tie the game up and move it into overtime. It may seem strange to think that these two diverse pictures could both inspire me or have anything in common, but they do.
Like many people, I am amazed and inspired by Lincoln’s life, rising from abject poverty, loss of his mother and beloved sister at an early age, an adversarial relationship with his father that he eventually escaped. As a young lawyer he developed lifelong depression that was so bad his doctor noted, “He was within an inch of being a perfect lunatic for life.” At one point his friends hid sharp objects and guns from him and Lincoln himself noted, “I am now the most miserable man living. If what I feel were equally distributed to the whole human family, there would not be one cheerful face on the earth.” In the midst of this, Lincoln suffered political defeats and all kinds of personal abuse, but found a profound sense of purpose in the antislavery issue and that sense of purpose and meaning propelled him to the presidency, and immortality, against great odds.
I recently read Doris Kearns Goodwin’s book “Leadership in Turbulent Times,” in which she describes Lincoln’s form of leadership as “transformational leadership,” that is, leadership that focuses on future goals and purpose rather than more expedient “transactional leadership.” In the many books that I have read about Lincoln I’ve come to see that Lincoln’s transformational leadership applies not only to leading those around you towards a greater good, but, perhaps more importantly, it is an internal leadership that lifts us as individuals to lives of meaning and purpose. Martin Luther King, Jr. famously said, "The arc of the moral universe is long, but it bends toward justice," and though it would be a century before that quote was spoken, Lincoln surely felt that same certainty, in part from his faith, but also from a deep confidence that he possessed the skills and determination to make a difference, just as each of us can in our own lives.
Johnny Unitas was from humble origins as well and early on nothing about him seemed remarkable or destined for greatness. Just three years before he played in that epic championship game, he was working construction and playing semi-pro football for six dollars a game. His sheer determination, confidence and quiet leadership were the hallmarks of his career. On that particular day, in an instant frozen in this photograph, he was poised to launch a long pass. 60,000 eyes would be pointed skyward while in the quarterback’s heart there was not only hope, but also a sense of certainty that the arc of the pass and the receiver sprinting downfield would connect in just the perfect spot, at just the perfect time. But more importantly, what inspires me when I look at the picture is the sense that there was also a certain kind of faith and resilience, a confidence that even if that particular pass fell to the ground, they would pick themselves up, huddle up and try again. There was an unspoken sense that his leadership, optimism and love of his work could make all the difference, attitudes critical in our own lives as physicians.
Who inspires you?
Brian S. Sayers, MD
Chair, TCMS Physician Wellness Program
Submitted March 12, 2019

A Surgeon’s Wellness Instruments: Empathy, Scalpel, and Music
Music has a primal power to impact quality of life whether it creates healing, happiness, self-expression, human connection or calm. Austinites, as listeners and performers, know that as well as anyone. Most of our lives are imbued with music; in restaurants and retail shops, in our cars and trucks, our late-night watering holes. We play music and it takes us away, to re-connecting, remembering, re-energizing.
When we are ailing, music can be soothing or pleasantly distracting and help with pain or worries. When most of us walk into a doctor’s office, our blood pressure rises about 10 points, our heart rate rises, and we feel anxious. When we are told we need surgery, that is a whole other level of stress. Music plays a big role for both my patients and me in the operating room. It can provide connection and calm.
After I talk with a person and examine their shoulder, elbow or hand, I arrive at a diagnosis. If I feel surgery is truly the best option for them, I recommend it. And then there is a pause, a reflection and a moment of wonder. I am always moved by my patients’ sudden and extreme faith. It is as if they are saying, “I just met you like 15 minutes ago, but sure, cut open my body. Take saw blades, scalpels, drills, screwdrivers, and chisels to me as needed. Whatever you think.” I am humbled by their trust. At the same time, I see “healing with steel” as actionable empathy. As surgeons, we listen, hear, see, understand, enter and attend. With this primal connection, this precise and sensitive action, we can alter the quality of a life.
On the day of surgery, I greet my patients on the gurney, and I can see the anxiety in their eyes. I say, “I know you’re worried, but I am confident that the surgery will go well ,and you will feel much better.” Then I say, “I always play music when I’m operating. You may not remember much of it, but what would you like to hear?” They always perk up with this. Most often, they say, “Whatever you want to listen to; I want YOU to be relaxed.” I tell them, “I like almost everything. And I’m always relaxed in the OR. It’s my happy place.” Then I might hear, “The Beatles!” or “I’m a classic rocker” or “classical” or “anything except what my 17-year-old plays these days . . .” This choice, this brief moment of control, this conversation about music, just before “going under,” has a calming effect.
Despite being in practice for over 20 years, I am continually inspired and intrigued by people’s stories; what they do, how they live, who and what they love. In addition to diagnosing their medical concern, it is so fascinating to learn what makes someone tick or creates a lift– the Talking Heads, fly-fishing, angel hair pasta, the banjo, rock climbing. The music they love.
O. Alton Barron, MD
Dr. Barron is an orthopedic surgeon with ATX Orthopedics and is a
Clinical Associate Professor of Orthopedics at Dell Medical School
Submitted January, 2019
Maybe It's Time
During the holidays I was running some errands, half
listening to a rerun of some financial show on the radio. I was mostly ignoring
it but then they said a couple of things that got my attention. One was that
time honored disclaimer “Past performance does not necessarily predict future
results,” followed by “the best way to predict the future is to create it.” Both
are rich material but the second one, a well-known quote attributed to Lincoln,
caught me at just the right time.
The transition from one year to the next is often a
time when we might become somewhat introspective about where we are in life,
how we might improve things, and what we need to leave behind. Positive change
requires careful assessment of what our current state of existence is, then the
difficult task of deciding what to shed, and what form transformation might
take. Sounds exhausting. You might think that the only things that need to be
shed are bad habits, or things that clearly work against our happiness and success.
You might be wrong.
In the world of business and organizational
development, “change management” is a critical component of success and is now
a well-established discipline in that world. Large organizations have executives
whose entire job is to help the organization evolve and survive by
strategically planning how to take a successful organization and pump new life
into it every few years. It is a critical key to long term survival.
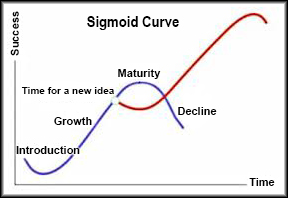
As I considered this, I reread Halftime by Bob Buford. A couple of the themes in the book are
interesting to think about. The first is “the sigmoid curve.” Organizations
that get off the ground and do well go through a fairly predictable cycle of
formation, development, growth, then the pinnacle of success, but then an
equally predictable decline if change is not part of the organization’s culture
− if it does not, or cannot, evolve. Once that decline begins it is hard to
reverse. You need look no farther than Sears, Toy R Us, shopping malls, bank
lobbies, World Book Encyclopedia and other bygone successes that are failing or
breathing their last gasps. The sigmoid curve holds that the time for change is
during the height of growth and success − before decline − while there is still
creativity, enthusiasm, and resources to bring about change that will
perpetuate success. It is profoundly counterintuitive as it calls for the
organization (or individual) to leave behind some of the things that actually
created success in the first place in order to achieve more lasting relevance. Buford’s
second point is that this constant, difficult evolution in people, is
ultimately an evolution “from success to significance.”
Most physicians are highly successful in their
practice, but how many go on to achieve not just success but also significance, and not just in their work
(which is no small thing), but also in something that transcends work and is
all encompassing in their own lives and in the lives of those around them? This
kind of change is not about giving up core values and beliefs, things that are
timeless and help us weather life’s storms, but is more about defining
priorities, how we go about our work, who we work with or for, and how we
nurture and cherish family and friends. Ultimately, it is about how we embrace
change at each unique stage in our lives, in order to fill our lives with
meaning, generosity, and love that spills over into the world around us. That
kind of change is the difficult work that defines our lives.
It may seem odd to quote Bradly Cooper, and this will
probably (hopefully) be the last time, but as I was writing this I happened to
hear his song from A Star is Born. It’s
not exactly Shakespeare but it’s a fitting thought to close with.
Maybe it's time to let the old ways die.
Maybe it's time to let the old ways die.
It takes a lot to change…
Hell, it takes a lot to try.
Maybe it's time to let the old ways die.
Brian S. Sayers, MD
Chair, TCMS Physician Wellness Program
Submitted November, 2018
True North

My oldest child is grown now with a career and a growing family, but he used to just be a kid, and like all children, he needed a bedtime routine. All too soon he lost interest in bedtime stories but we still needed a way to wind down together at bedtime. In those days a set of encyclopedias was still on the shelf and for a while we ended the day exploring the world together in those books. We would randomly select a volume, then flip it open read about whatever was on the page we landed on. It’s surprising how many of those random facts I still remember today. One evening we read about “true north.”
I always thought that a compass points to the North Pole. Like so many other things, I was wrong. True north is the direction along the earth's surface towards the geographic North Pole. It is almost identical to astronomical true north, calculated for centuries by ocean bound navigators. It is a static, predictable point mariners have depended on since man began to travel.
Magnetic north is a wandering point in the northern hemisphere where the planet's magnetic field is vertically centered. It is the direction compasses point. Magnetic north varies slightly from year to year, altered by natural and man-made magnetic fields. Following magnetic north as a navigation strategy over long distances to precise points will inevitably cause us to become lost, as ancient mariners knew.
And so all these years later, this fun fact I learned with my son one evening returns to haunt me (and now you) as a metaphor. In life's journey we are often uncertain where we stand, where we are going and what is the right path. True North is the internal compass that guides you successfully through life. It represents who you are as a human being at your deepest level. It is your point of orientation - your fixed point in a spinning world - that helps you stay on track as a leader and as a human being. Your True North is based on what is most important to you, your most cherished values and beliefs, your passions and motivations, the sources of satisfaction in your life. Ignoring or leaving True North unexamined is dangerous and can rob life of meaning. Finding and following True North is the difficult work that defines our lives.
When it comes to vocation, we might consider True North as another way of describing our calling—how we match what is deep within our heart and the unique gifts we have been given, with what the world cries out for in need.
I speak to physician groups frequently about burnout and wellness, and many times I have flipped through my well-worn power point slides about both. More and more it occurs to me now that most of these slides are ultimately useless unless we as individuals spend more time exploring, discovering and then tenaciously following our own unique True North.
Most of us were in small practices when my career began, now 70% of physicians are employed. Often, our professional lives are influenced, if not controlled, by people far removed from the realities and sacredness of the exam room. To practice in an environment that ignores the importance of things like calling, relationships, values, respect and meaning, instead focusing most visibly on profit and market share, devalues the humanity in our work and its wake can land us as individuals onto a rocky shoreline before we even realize we have strayed off course. Self-examination in medicine these days requires not only examining what is deep within us, but also what we allow to go on around us. If our own values and calling are in conflict with the practice or organization we work within, we go to work each day in great personal peril. Fortunately, we have some great leaders in our medical community, many of whom support the Physician Wellness Program, who are increasingly committed to physician wellbeing. Be a voice within your organization. Watch out for your colleagues. We still have a long way to go.
Brian S. Sayers, MD
Chair, TCMS Physician Wellness Program
Submitted September, 2018
The Cloud of Witnesses

During my years in study at an Episcopal seminary, I came to appreciate the reverence Episcopalians have for the saints. There are hundreds of recognized saints and one semester I spent several months studying some of their life stories and the spiritual gifts they left behind. The Old Testament refers to the "cloud of witnesses," the faithful who pave the way for subsequent generations. Of course, the importance of the heritage of important figures in inspiring and giving us direction is not unique to religion. As Americans, we venerate the founding fathers, Lincoln, King, and many others. There are legendary athletes that sports fans compare modern day athletes to, as well as educators, authors, scientists, social activists. Imperfect as they were, their life stories are guideposts of inspiration. Medicine is no exception. Lister, Curie, Freud, Fleming, Jenner, Osler, DeBakey, and so many other giants along with the teachers and mentors who paved the way for us. The cloud of witnesses is sometimes likened to the crowd that cheers you on as you run a marathon or 10k. Often nameless and faceless, but full of those who care about us, want success for us, cheering us on.
For the last few years, I have had the honor to write memorials in the TCMS Journal for our departed colleagues. Some were well known to me, others I never met. Given the generation now passing, most are male, almost all served in the military, the majority trained in Texas or the south. The women of that generation who have passed serve to create a very special witness to our profession, their unique obstacles as women in medicine in that era an especially rich heritage. As I piece together their lives, not surprisingly what stands out more than the accomplishments that punctuated their lives is the heritage of compassion, accessibility, friendship, and faithfulness they imbedded in the hearts of the lives they touched. Poet David Whyte notes, "Death is not impressed by what we have done, unless what we have done leaves a legacy of life...what is remembered in all our work is what is still alive in the hearts and minds of others.” I often think of doctors who I have worked with, along with mentors and teachers who are gone now but gave me gifts that I still call on today. They likely had no idea that I would see things in them that I would carry with me that make me a better doctor and a better man.
We accomplish much in our lives as doctors. We make lives better, cure or control disease, and, on a good day, even connect with patients and bring real healing, often against great odds. We should not lose sight of the fact that connecting with colleagues, being available to listen and advise, to be an encouraging and compassionate presence, is one of our primary callings and ultimately is the most important thing we leave behind to our colleagues and our profession.
These are difficult times to practice medicine. We know that burnout is all around us – statistically about half of us – and not just the usual irritations of work but true burnout with life altering effects that shade all phases of our lives as well as impacting patient safety. Keep an eye out for colleagues who may be struggling, check in with them, encourage them to get help or at least talk about it. Realize it or not, your life is an example to those around you and there are unseen opportunities to help your colleagues who may need help but don’t get it out of shame or denial.
Brian S. Sayers, MD
Chair, TCMS Physician Wellness Program
Submitted July, 2018
The Hero’s Journey

Since childhood, one of my favorite stories is David and Goliath, the story of the young, future king who finds himself – by a combination of chance and choice – facing the Philistine giant. The fate of his army depends on him alone, with only his wits, faith and courage to perform a seemingly impossible feat. We might all identify with this story, as we have all felt ourselves to be an underdog at some point in our lives. As I was preparing a class about this story recently, I came across an essay about the “monomyth” or “The Hero’s Journey.” Described by author Joseph Campbell and others, the Hero’s Journey is a basic story pattern throughout mythology, a pattern frequently found in other ancient writings as well as later day literature and film.
A very brief summary of the stages of The Hero’s Journey is as follows: the hero from the ordinary world is called to adventure. After initially refusing the call, he crosses the threshold into a supernatural region. He descends into “the belly of the whale” and “the road of trials,” along the way meeting with helpers, mentors, a goddess, a temptress, and seemingly insurmountable challenges. There is atonement with a higher power, then receipt of the boon (treasure) and apotheosis (achievement of a higher level of existence), finally rebirth and return to the ordinary world, now possessing gifts to bestow on humanity.
Literature is often a reflection of everyday life, and if we spend a little time thinking about it we may be able to see many small, and perhaps a few large, monomyths in our own lives. Our lives in medicine these days is easily seen through this lens. We pass through a certain threshold from our early lives into a life of medicine, lives that are full of mentors, challenges, temptations and perhaps dark times spent in the “belly of the whale.” But like the heroes in many of the stories, as we navigate difficult times the treasure that we acquire may be a certain kind of knowledge, perhaps even wisdom, a boon that we are called to share with our colleagues and all of humanity, one patient at a time. To achieve and then share the gifts that we attain on this journey is indeed heroic, anything but ordinary, but often obtained at great cost.
Different authors describe The Hero’s Journey in different terms, but all include the importance of the “mentor” or “supernatural aid” that assists in the journey. We may find this assistance in several ways. One is deep within our own souls, beyond ego where our deepest desires and meaning lives, a place it takes some effort to reach. Another is found within our community of colleagues, bound together with common hopes and goals, supporting each other, sometimes going arm and arm down the “road of trials,” then hopefully beyond it. Lastly, there is something woven within, but also beyond, both of those. On my desk I have a fortune from a fortune cookie with a well-known saying: “Act boldly and unseen forces will come to your aid.” The ambiguous sounding “unseen forces” is open to individual interpretation. In my own life it means something very specific, but beyond that, the saying is significant in calling on us to whine and retreat as little as possible in the face of life’s important challenges, but rather to act boldly as we carry our gifts and dreams into a world in need, regardless of obstacles in our way, and to do so in a way that breathes life into us and those around us.
Brian S. Sayers, MD
Dr. Sayers is Chair of the TCMS Physician Wellness Program
Submitted April 30
An Endangered Species, or an Evolving Species?
In an article from the last issue of the TCMS Journal, Dell Medical School Dean Clay Johnston, MD, PhD, makes insightful observations about the future of practicing physicians and the mindset we will need to remain relevant. Are physicians, at least as we have traditionally considered ourselves, really an endangered species? He observes what many of us have already grudgingly concluded: that the capabilities of AI (artificial intelligence) will increasingly replace much of the data storage and problem solving tasks that physicians have traditionally seen as their own unique gifts. As this happens rapidly and predictably, what will be the role of physicians? Will that new role be an entirely new direction for us, or a return to the deepest roots of the healing profession?
Dr. Johnston notes that the way medical schools train physicians will need to undergo a sea-change to prepare the next generation of physicians: “Most allocate substantial time to memorization and analysis, tasks that will become less demanding as artificial intelligence improves. But components of the art of caring—communication, empathy, shared decision-making, leadership, and team-building—are underemphasized, when they are emphasized at all… It’s essential that medical education leaders rebalance their curricula toward these components. Doing so will help patients receive the best care that medicine and machine have to offer. It may be good for physicians as well, as they find more opportunities for meaningful patient communication and delivery of higher-quality care.”
Dr. Johnston notes, “We know that the art of caring is central to the medical profession.” Indeed, it is one of the few things that AI cannot replace. Physicians will need to remember that curing and healing are not the same and our call as physicians in providing care is to endeavor to restore wholeness to the person, not just the body.
How do we realign this mindset as a profession? Daniel Sulsmasy, in his article, Is Medicine a Spiritual Practice?, observes that for physicians to really connect with their patients they must be willing to explore, or at the very least acknowledge, that patients struggle with “the big questions. What is the meaning of my illness? Why must I suffer? Is there anything about me that is valuable now that I am no longer ‘productive?’... Can my doctor possibly understand what I am really going through? A physician who has begun to explore these questions in his or her own life will be better prepared to help patients struggle with these questions.”
Brian S. Sayers, MD
Dr. Sayers is Chair of the TCMS Physician Wellness program
Submitted March 28
The Medical Marriage

Adam Taylor/ABC via Getty Images
First the good news. Contradicting earlier studies with potentially flawed designs, a study out of Harvard that looked at data from 6 million people, including 40,000 physicians, found that physicians, 27% of whom reported ever being divorced, are actually less likely to divorce than the general population of non-healthcare employed people, 35% of whom had been divorced. Broken down into healthcare professionals, we stack up well again, less likely to have experienced divorce than dentists, healthcare executives and nurses.
In spite of this good news, married physicians face unique challenges to be navigated. Our work as physicians can be highly stressful and involve long hours physically (or emotionally) away from our families. We often bring these stresses home with us. The traits that can make us excel as physicians as often as not may make us a challenge to be married to. Women in medicine often face an additional set of challenges balancing work and family life and are 1.5 times more likely to have been divorced than their male counterpart of similar age, with women physicians working more than 40 hours per week at particular risk.
So what is the key to a successful medical marriage? A number of strategies have been suggested. One study from Mayo Clinic looking at factors that work for and against the medical marriage from the spouses vantage point demonstrated that “on multivariate analysis, minutes spent awake with their physician partners each day was the strongest predictor of relationship satisfaction, exhibiting a dose-response effect.” Other studies have also identified time together as the key, although at least one has demonstrated that quality time is really the key with spurts of just 30-120 seconds of “caring interaction for a total of 20-30 minutes a day,” to be a key predictor of marital success (Sotile/Fraenkel). By any measure, time with your spouse is a critical ingredient, also one very difficult to navigate when so much time and emotional energy are consumed by career and the “parenting vortex.”
In April, the TCMS Physician Wellness Program is proud to add a Certified Gottman Couples Therapist to our coaching panel for couples in need of expert help in making their marriage the best it can be. Here is more information about couples coaching as well as our coaching program.
Brian S. Sayers, MD
Dr. Sayers is Chair of the TCMS Physician Wellness program
Submitted March 5
When 20% is a Passing Grade, but Surprisingly Hard to Get
Last fall I attended a nationwide conference on physician burnout and resiliency in which a researcher from Mayo Clinic presented data about causes of physician burnout. In the study, they looked at certain characteristics of physicians who fulfilled criteria for burnout and those who did not and tried see how the two groups differed in certain categories
They asked participants to identify what work related activities they find most meaningful. Examples included direct patient care, administration, research and education activities. They found that physicians who spend at least 20% of their time on their most personally meaningful activity have a burnout rate that is half of those who spend less than 20% of their time on favored activities. It is, of course, both amazing and frightening to think how many physician fall short of that low percentage in their workday, but not surprising what the consequences are.
Shortly before I sat down to write this, I listened to a podcast during a run that featured Shawn Achor, an expert in positive psychology. In describing the “secrets of happiness” he notes the importance of redefining how we think of happiness. His argument is that if we define happiness only in terms of pleasure or the final accomplishment of a goal, then happiness is never more than a fleeting moment in time. He calls on us to see happiness as primarily being “the joy we feel while striving towards our potential.” The potential he refers to is our ultimate capacity for optimizing relationships, vocation, and other integral aspects of our lives. Intimately linked to realizing joy and happiness, he argues, is a sense that the things you are involved in have meaning.
As we try to navigate our professional careers towards happiness and fulfillment, an important call is to recognize what part of our work is most meaningful to us and to make sure that in the course of a normal workday that activity is consistently and proportionately represented.
What specific activity is most meaningful to you? How well is it represented in a typical day?
-Brian S. Sayers, MD
Dr. Sayers is Chair of the TCMS Physician Wellness program
Submitted Febuary 2
Healing From Within
I have been an internal medicine physician for over two decades
and have traveled the world both as a missionary physician and a tourist. When
I am home in the United States, I can feel a palpable and growing level of
stress in our communities across America, as evidenced by the ever-increasing
opioid crisis, alarming rates of obesity, rising statistics of violence,
depression, and sadly, suicide. This level of stress is much higher in the
United States than other countries I visited. I have felt helpless for many
years, not really knowing how to treat my patients facing stress-induced diseases.
How could I? Like many of my colleagues, I was practicing with burnout symptoms
for many years.
Then, in 2009, I had a personal tragedy so horrific that I knew
prescription medicine could not help me to heal. I had to find a different way.
I was encouraged to try meditation. Despite my skepticism, I decided to put
effort into the daily practice of meditation. To my surprise, it worked. It not
only took away the emotional pain and burn-out symptoms but replaced it with a
deep joy that is difficult to describe.
This led me into research for the next several years on why and
how meditation heals. What I found was substantial research in meditation in
major universities throughout the United States, particularly at the University
of Massachusetts and Harvard Medical School. Meditation is offered as treatment
for many conditions including hypertension, depression, anxiety, ADD/ADHD, just
to name a few. Meditation reduces complications to chemotherapy, radiation
therapy, AIDS treatment, surgeries, and the list goes on and on. Meditation
works because it counteracts the stress response creating a relaxation response
that allows the body to heal. It is now considered a significant evidence-based
practice in medicine.
Meditation is currently widely used in many occupations. It is
being adopted in the military for stress and resiliency. In the corporate
world, companies such as Google, have incorporated meditation into the work day
as it has shown to improve morale, focus, less sick days, and increased
productivity. Schools are using meditation instead of detention, showing
improved attention, behavior, and grades. Even in sports, professional football
players and Olympians use meditation daily to help their focus.
I practice a meditation called the Centering Method, a
mindfulness meditation. It is a simple method that elicits the relaxation
response when practiced daily. I brought this meditation practice to physicians
in 2014. We now have ongoing workshops at setoncove.net.
Meditation has been practiced for thousands of years. However,
we have only started to study its benefits. I see a future where we learn that
the power of healing is truly within each of us.
Anna Vu-Wallace, MD
Dr. Vu-Wallace is a hospitalist and is
founder of the Mindfulness Meditation Clinic at Seton Cove
Submitted December 31
Thresholds
The
beginning of each new year often becomes a sort of artificial but important
threshold, a time when we look back on the old, both regrets and joys, and wonder
about the year to come. Some years when happiness and abundance have marked our
year the transition is easy, almost entirely unexamined, while other years,
recent events of loss or regret challenge us toward self-examination and
change. To acknowledge and navigate significant change, a threshold, in any
meaningful way requires honest reflection and courage. The late poet John
O’Donohue commented on such times of challenge:
“To
acknowledge and cross a new threshold is always a challenge. It demands courage
and also a sense of trust in whatever is emerging. This becomes essential when
a threshold opens suddenly in front of you, one for which you had no
preparation. This could be illness, suffering or loss. Because we are so
engaged with the world, we usually forget how fragile life can be and how
vulnerable we always are. It takes only a couple of seconds for a life to
change irreversibly. Suddenly you stand on completely strange ground and a new
course of life has to be embraced. Especially at such times we desperately need
blessing and protection. You look back at the life you have lived up to a few
hours before, and it suddenly seems so far away. Think for a moment how, across
the world, someone’s life has just changed – irrevocably, permanently, and not
necessarily for the better – and everything that was once so steady, so
reliable, must now find a new way of unfolding.”
Sometimes
thresholds are abrupt and dramatic as O’Donohue describes. More often, arrival
at one of life’s thresholds is more subtle, but no less profound and
challenging to discern and cross. In such times, we need to call on not only
the invisible strength found within us, but also the support available from
those around us, to produce visible and productive change. As he goes on to note
in his poem “For the Interim Time,”
during such times,
“What is being transfigured
here is your mind
And it is difficult and slow
to become new.
The more faithfully you can
endure here,
The more refined your heart
will become
For your arrival in the new
dawn.”
We hope the old year
ended with happy memories, gratitude, and professional satisfaction and that
the New Year will be full of family and friends as well a sense of purpose and
meaning in your work. If you find yourself in a time of challenge and in need
of help, please consider reaching out to the PWP confidential coaching program,
where one of our professional counselors is only a phone call away.
-A physician
Submitted November 29
It’s the Most Wonderful Time of the Year (?)
In the midst of digging out of the colossal mess left over from our great family gathering at Thanksgiving, then bringing down the seemingly endless boxes of Christmas decorations from the attic to sort through, I convinced myself it might be therapeutic to read about survival/enjoyment during the holidays. Here’s a few of the most common tips:
- Gratitude. Expressing gratitude on a daily basis and in tangible ways (verbally or in writing) is incredibly powerful. There is a whole body of literature about the measurable and life changing mental health benefits of this practice. Spend a little time reading about it or look at some links and videos about gratitude at tcms.com/Education-Resources.
- Reconnect with your faith or spiritual practices. Plan out quiet time, walks, reading sacred texts, poetry or other inspirational writings or find time for worship and thanksgiving.
- Reconnect with family and friends, and not just texts and emails but something relaxed and unrushed. If they are not nearby, surprise them with an actual phone call. If they are close by, share a meal or meet for coffee or do something without a lot of time pressure.
- Avoid toxic people or situations. You know exactly who and what this means. Enough said.
- Enjoy some unscheduled, unstructured time. There is great power and rejuvenation in the fine art of “goofing off.”
- Unplug. Find time when someone else is on call to turn off your phone, your computer and forget the emails. You might just have a chance to get to know yourself, your family or friends with distractions missing.
- Go outside. Take a “nature bath.” There is surprisingly robust research about the mental health benefits of spending time in nature.
- Take care of yourself. Holiday food and drink is everywhere. A little moderation and some exercise won’t kill you.
- Forget about finding the perfect gift. It doesn’t exist. As you fret over gifts, reconsider generosity. Be generous with your time and your love.
- Keep a mental scorecard. Which one is leading, the “stuff” or meaning and connections? If the stuff gets too far ahead, it might be time for a coaching change.
Can this be the most wonderful time of the year? Absolutely! It should be full of family, friends, fun, rest and meaning. It just takes the right mindset and maybe the ability to pause and take a deep breath every now and then.
If are struggling and think you might need a little help, consider calling the 24-hour confidential PWP coaching hotline 512-467-5165 and we will help you connect with one of our TCMS counselors by phone or in person.
-Happy Holidays!
Submitted November 7
On Being Perfect
Compulsive, perfectionist. Personality traits often blamed as root causes of physician burnout. There is a part of perfection seeking that makes us better doctors, but another part that can be profoundly destructive. When we fall short of our own expectations, either through our own missteps or because of things we cannot control, with the wrong mindset it can send us into a spiral of self-doubt, hesitation or defensiveness that impairs our ability to provide good care for patients, and ourselves.
No matter how hard we try, sometimes things go wrong. It is part of our lives in medicine, life in general for that matter, which goes against our quest for perfection, a quest we take on in equal measure for our patients and our egos. At some point we have to come to terms with imperfection, with failure, and see these events for what they are and what they teach us and at some point redefine what perfection really means.
I am a sucker for old sports movies as they study not only those who succeed, but also those who seemingly fail. My favorite scene in Friday Night Lights is the halftime pep talk that the coach, played by Billy Bob Thornton, gives during their championship game:
“…You got two more quarters and that's it. Now, ya'll have known me for a while, and for a long time now you've been hearin' me talk about being perfect…To me, being perfect is not about that scoreboard out there. It's not about winning. It's about you and your relationship to yourself and your family and your friends. Being perfect is about being able to look your friends in the eye and know that you didn't let them down, because you told them the truth. And that truth is that you did everything that you could. There wasn't one more thing that you could've done… Can you live in that moment, as best you can, with clear eyes and love in your heart? If you can do that gentlemen, then you're perfect.”
As physicians, perhaps we should learn a lesson from the coach, redefine perfection and know you can achieve it, regardless of the outcome, when you can look into the eyes of your patient, and into the mirror, and can truthfully say you did everything you could, there wasn’t one more thing you could have done, and say it with clear eyes and love in your heart.
-A physician
Submitted October 6
Compassion
I was the senior resident in the ICU. It was late and I was
exhausted. A sleet storm was in progress outside the hospital and miles away in
a remote area in far northern New Mexico a blizzard was in progress. Somehow Life
Flight had managed to get out ahead of the storm and transported Roy to County where
he landed on my service. He arrived in cardiogenic shock with ominous tall,
wide ST elevations that we identified as “tombstones,” signifying what in those
days would as likely as not be a fatal event.
The usual frenzied dance followed, using protocols that sound
primitive now, all the while knowing his chances were slim. He rallied after I had
sent the interns and students off to get a little sleep, was even oriented and
conversant for a while before the arrest and futile code. He told me about his
ranch, snow covered now, but soon, in the spring, lush green pastures would
re-emerge in a valley below two tall mountains, snow fed streams coursing through
the valley. A family ranch where his wife was now stranded in the storm, and
where tomorrow his son would have to try and drive the pickup into the pasture,
his grandson pushing square bales out into the snow for the cattle as they went
along. The old man’s face was pale, deeply creased, sun damaged, and now with
tears. I think that night was the first time I held a patient’s hand for more
than an instant, in this case for an hour or more, his hand clutching mine at
times. By 7:00 a.m. my shift was done, and so was Roy. I called his wife then
headed home, and slept.
We have talked about physician wellness a lot lately and it
occurs to me that at the core of it lies compassion, of sharing the suffering
of others. Burnout and compassion travel against each other with opposite trajectories,
one always ahead of the other. Our lives in medicine are defined by compassion,
both in giving it, but also in feeling worthy of receiving it. We might ask
ourselves many times in a long career, “How do we nurture and protect it?” Without
compassion, we are just technicians.
Even today I will sometimes see a cardiac monitor in the
unit and think of Roy. Most years, driving to a favorite spot in Colorado I
will pass by a certain wide pasture, emerald green, framed with tall mountains,
dotted with cattle, and pray that I will never forget that night.
-A
physician
Submitted September 5, 2017
The Inner Environment
For physicians who go through a period of dissatisfaction (or worse) with their work, there is a tendency to blame external factors. This is encouraged by countless articles and books written about physician burnout in recent years. It is hard to ignore the factors that seem to conspire against us. The systems we work in that sometimes appear to be as concerned with production as with quality, the avalanche of regulatory requirements, and the disproportionate amount of time we spend with EMRs and wrestling with insurers. All of these things, and many others, take us away from the one thing that physicians value most in reflective moments – unpressured time to have meaningful, human interaction with their patients. True as this might be, at some point we may have to realize that while there are “systems” problems in our work that we cannot control, what we can control is how we react to these potentially destructive forces, and in doing so, we just might preserve a sense of joy and meaning in our work. Controlling how we respond takes hard work, perhaps the hardest kind. It requires that we look inward.
Ronald Epstein, author of Attending: Medicine, Mindfulness and Humanity, and our 2017 TCMS Foundation Lecturer, speaks of this in his book: “Burned-out physicians are not only alienated from patients; they are also alienated from themselves…. But changing the health care system won’t solve it all. It is important to recognize that burnout has affected clinicians for centuries, and important causes of burnout reside within clinicians themselves. For the first time in memory…some doctors are finally paying attention to their inner environment in a systematic way and finding ways to bring greater presence and resilience to the practice of medicine.”
Paying attention to what Dr. Epstein describes as the “inner environment” is a unique process, requiring skills, patience and self-examination that does not come naturally to most of us, but the rewards for us and our patients can be immense. It is work that leads to the meaning and connection in our daily lives that we always assumed awaited us when we put on that first white coat.
-A PWP committee member
Submitted: July 20, 2017
During the past year I have been a part of a couple of physician wellness workshops in which one of the speakers uses an exercise about our calling to be physicians as an ice breaker.
She asks members of the audience to turn to one or two people sitting next to them, preferably someone they do not know well, and tell the story of how you decided to become a doctor. It is a little awkward telling someone you don’t know something about you that is potentially either a fairly
personal story, or one that might just sound lame, or a story you can’t fully put into words. Over the years, patients have asked me often enough why I wanted to be a doctor and I reply with something very brief and unrevealing−more of a sound bite than a real explanation. But with a colleague, and
in this type of setting, I have found that it does make me think more carefully, to recall complex feeling and events that led to the decision, and then share it with a relative stranger.
It does create an instant bond of sorts, perhaps even a new friend, something that is clearly part of the exercise.
There is also great power recalling and verbalizing the nature of that call all these years later.
The second part of the exercise is then to address the question, “Why do you continue to practice medicine today?” If the second answer is different from the first, and it often is, that is certainly food for thought. Is the sense of calling to medicine at our current stage of life one that energizes us,
fills our work with meaning, our lives with joy even in the face of challenge, or is it now a life of perceived drudgery and annoying obstacles? The answer may say much about how we interact with patients and loved ones, and whether strategies for change/renewal are needed.
Considering the need for a course correction might start with a challenge described by author David Whyte: “…try to imagine what that dreaming young self would think of the strange adult we have become.”
-A late career internist